Sickle Cell Retinopathy
Figure 1. Color retinography of the right eye: telangiectasias and areas of ischemia are observed in the temporal and superior mid-periphery, as well as iridescent patches.
Figures 2 and 3. Color retinographies of the left eye showing the presence of salmon-patch hemorrhages, telangiectasias, and peripheral ischemia.
Figures 2 and 3. Color retinographies of the left eye showing the presence of salmon-patch hemorrhages, telangiectasias, and peripheral ischemia.
Description
Sickle cell retinopathy is a progressive vascular condition caused by intravascular hemolysis and oxygen deficiency that occurs in sickle cell disease.
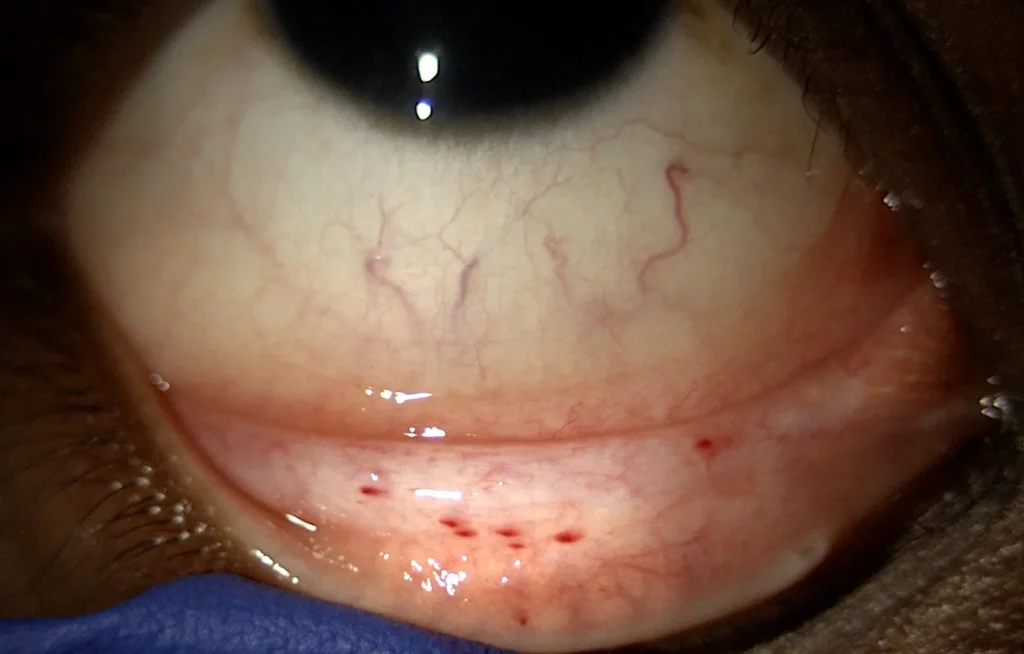
In initial stages, there is ischemia without neovascular proliferation. During examination, it is common to find conjunctival hemorrhages or petechiae, vascular tortuosity, an increase in the foveal avascular zone (FAZ), and the presence of characteristic retinal hemorrhages called “salmon patches”, due to the appearance they acquire from the hemolysis of red blood cells. These hemorrhagic lesions are absorbed, depositing hemosiderin, forming iridescent patches, which can cause migration and proliferation of the pigment epithelium, forming hyperpigmented lesions known as “black sunburst” or black sunburst.
In more advanced proliferative forms, ischemia triggers neovascularization, typically in a “sea fan” pattern, leading in severe cases to vitreous hemorrhage or tractional retinal detachment.
Systemic treatment reduces the risk of retinopathy progression and can even lead to regression of neovascular lesions.