Acute Middle Paracentral Maculopathy
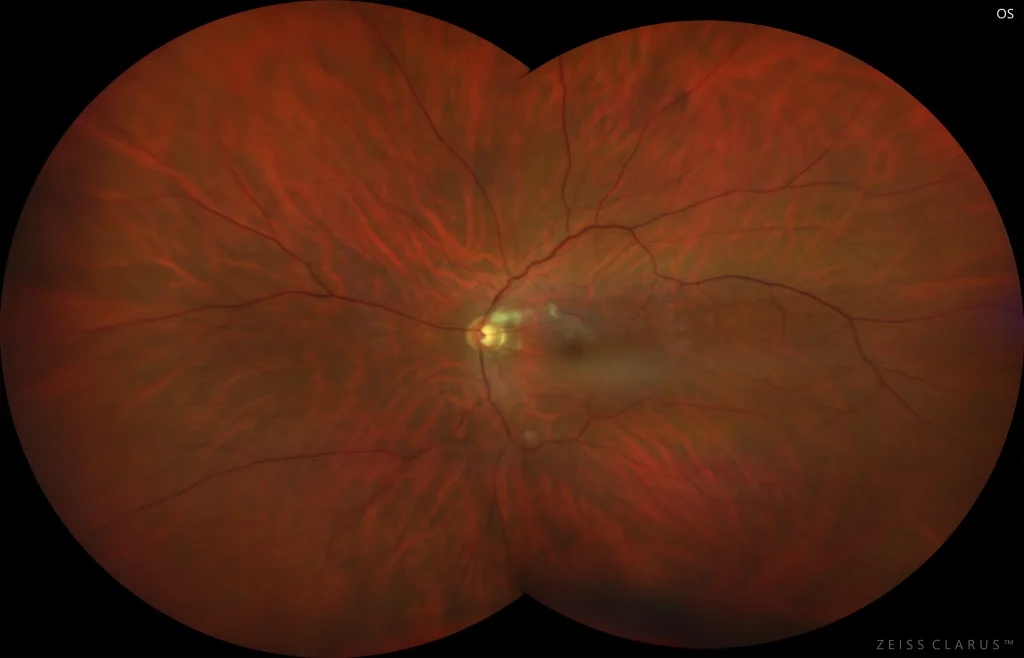
Figure 2. Color retinography of the left eye showing the presence of deep whitish lesions in the papillomacular bundle consistent with the ischemic area
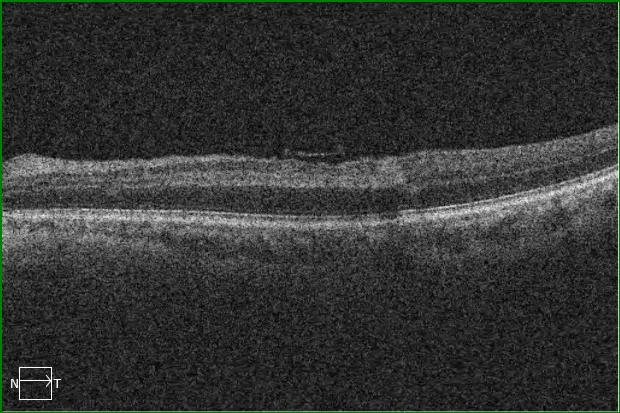
Figure 3. Optical Coherence Tomography of the left eye macula. Hyperreflective band in the superior juxtamacular region of the inner nuclear layer suggestive of PAMM
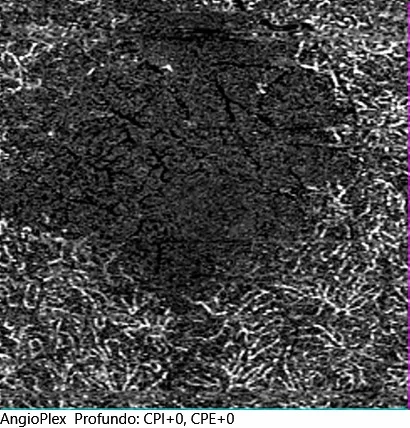
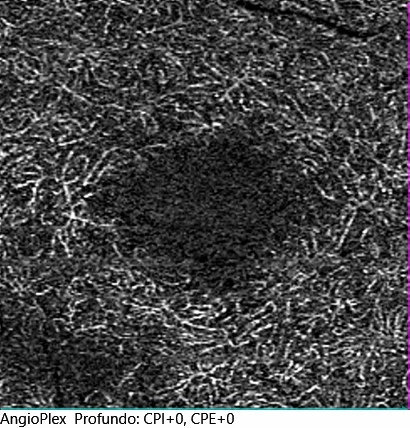
Figures 4 and 4'. Angio-OCT of the right eye and left eye deep plexus. Isolated ischemia of the superior juxtafoveal deep capillary plexus is observed in the left eye, corresponding to the affected area in the macular OCT
Description
Acute Middle Paracentral Maculopathy (PAMM) is an ischemic vascular occlusion of the middle retina due to involvement of the deep vascular plexus. Among its main risk factors are the use of oral contraceptives, coagulopathies, or any cardiovascular risk factor (diabetes mellitus, hypertension, etc.). It is imperative to conduct a study to rule out embolic causes, so the diagnosis should include imaging tests, cardiological and vascular studies.
The fundus may be normal or show deep whitish lesions with poorly defined borders, which can be confused with cotton wool spots. The image in macular Optical Coherence Tomography (OCT) is typical, as it presents as a hyperreflective lesion in middle layers (inner nuclear and junction zone between outer plexiform and inner nuclear). It usually presents with symptoms of a central or paracentral scotoma appearing.
It is possible to objectively observe the ischemia of the deep vascular plexus in angio-OCT and evaluate the scotoma with a visual field test. Generally, the prognosis is good and the scotomas reduce, although it is common for them not to disappear completely due to the atrophic legacy in the middle layers of the affected area.