Macular Atrophy
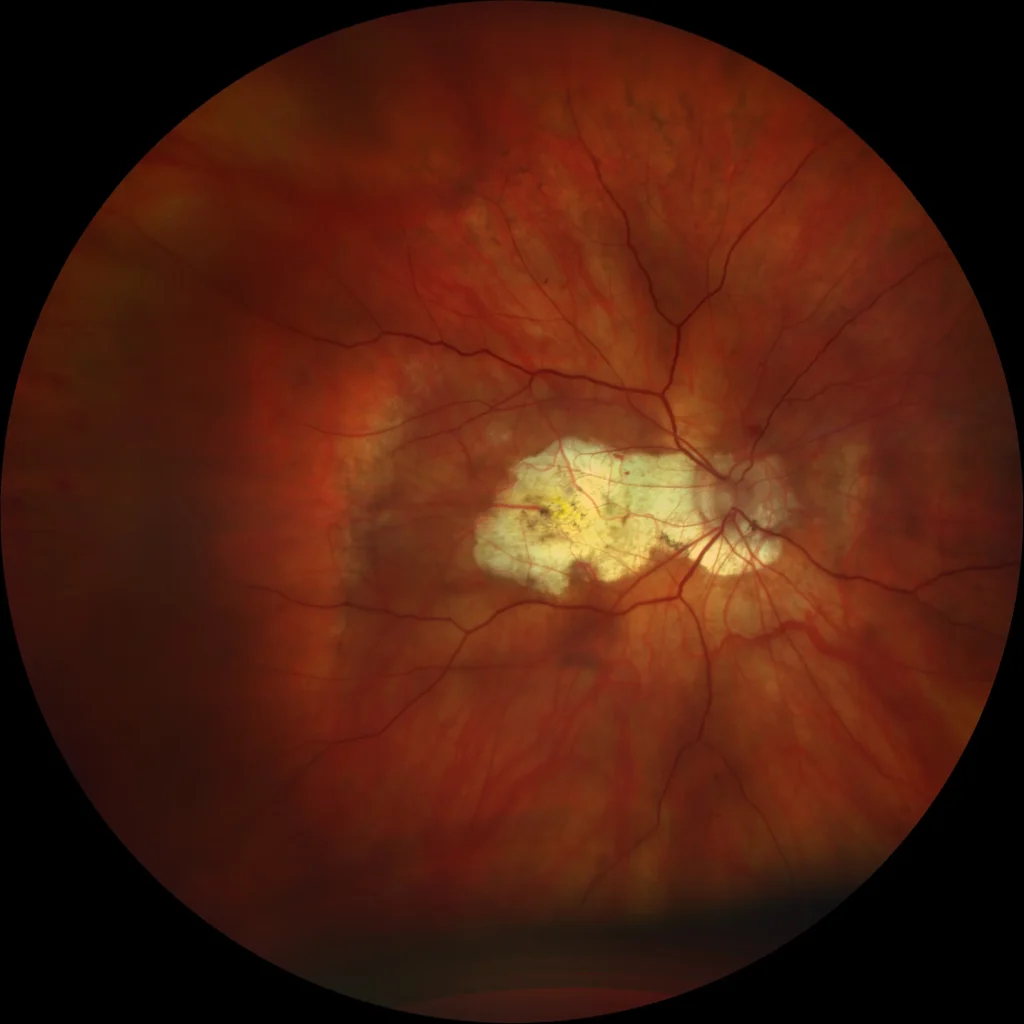
Color retinography (Clarus500, Zeiss): (A) OD: The image shows a chorio-retinal atrophy plaque extending from the optic disc to the macula. These plaques are well-defined and appear whitish due to the absence of retinal pigment epithelium (RPE), outer retinal layers, and most of the choroid, allowing the sclera to be visible through transparency.
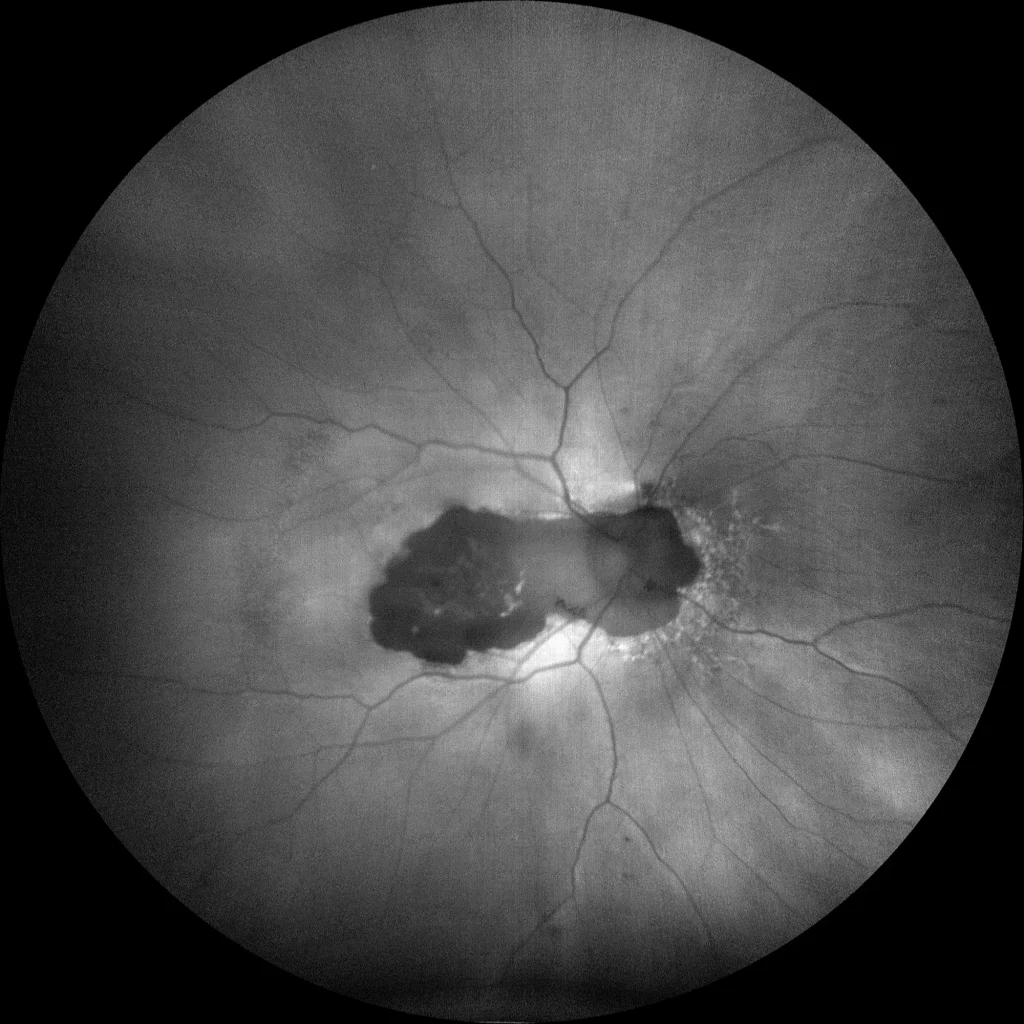
Autofluorescence (Clarus500, Zeiss): (B) OD: Hypoautofluorescent atrophy plaque extending from the optic disc to the macula. The hypoautofluorescence shows the absence of RPE in the area covered by the lesion.
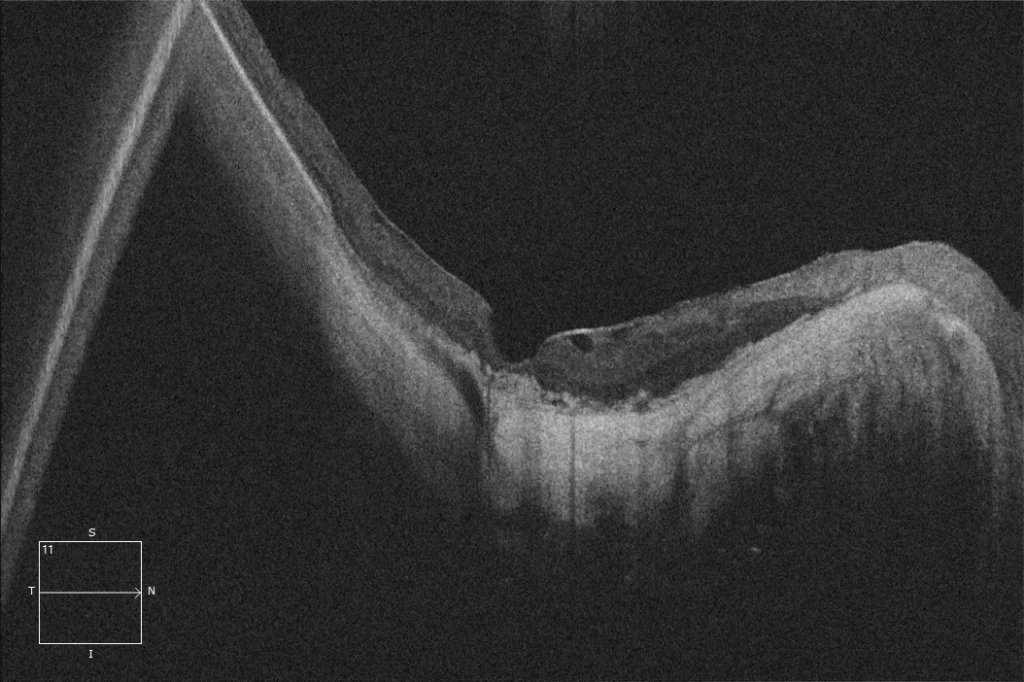
OCT (Cirrus6000, Zeiss) (C) OD: The OCT shows the presence of a marked posterior staphyloma with absence of RPE, outer retinal layers, and choroidal tissue in the macula, where the inner retina rests directly on the sclera. A hyperreflective epiretinal tissue can also be observed, which could correspond to an epiretinal membrane or remnants of a split posterior hyaloid.
Description
Presence in the macula of one or more atrophy plaques that manifest as focal, circumscribed, and well-defined areas of absence of RPE, outer retinal layers, and most of the choroidal thickness. Myopic macular atrophy can be caused by a myopic neovascular membrane or be the consequence of patchy atrophy progressing to the macula. This lesion is one of the main causes of vision loss below 0.1 in high myopic patients and corresponds to the most advanced category (stage A4) of the atrophic component of the ATN classification.
Comments
Minimum attached tests: Retinography + Autofluorescence + OCT- Color retinography (Clarus500, Zeiss): (A) OD: The image shows a chorio-retinal atrophy plaque extending from the optic disc to the macula. These plaques are well-defined and appear whitish due to the absence of retinal pigment epithelium (RPE), outer retinal layers, and most of the choroid, allowing the sclera to be visible through transparency.
- Autofluorescence (Clarus500, Zeiss): (B) OD: Hypoautofluorescent atrophy plaque extending from the optic disc to the macula. The hypoautofluorescence shows the absence of RPE in the area covered by the lesion.
- OCT (Cirrus6000, Zeiss) (C) OD: The OCT shows the presence of a marked posterior staphyloma with absence of RPE, outer retinal layers, and choroidal tissue in the macula, where the inner retina rests directly on the sclera. A hyperreflective epiretinal tissue can also be observed, which could correspond to an epiretinal membrane or remnants of a split posterior hyaloid.