Ocular toxoplasmosis
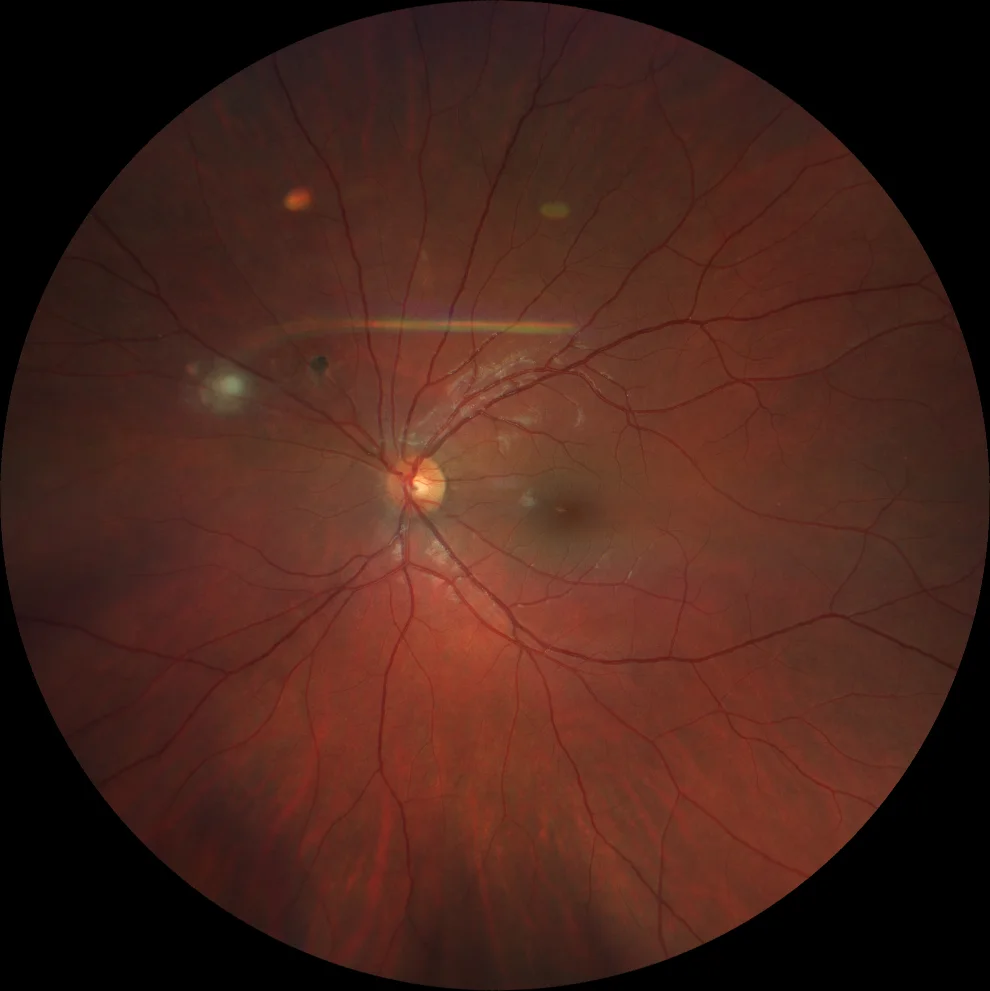
A. Color fundus (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye showing a hyperpigmented scar superonasal to the papilla and a more nasal focus of active retinitis, whitish in color with mild overlying vitritis.
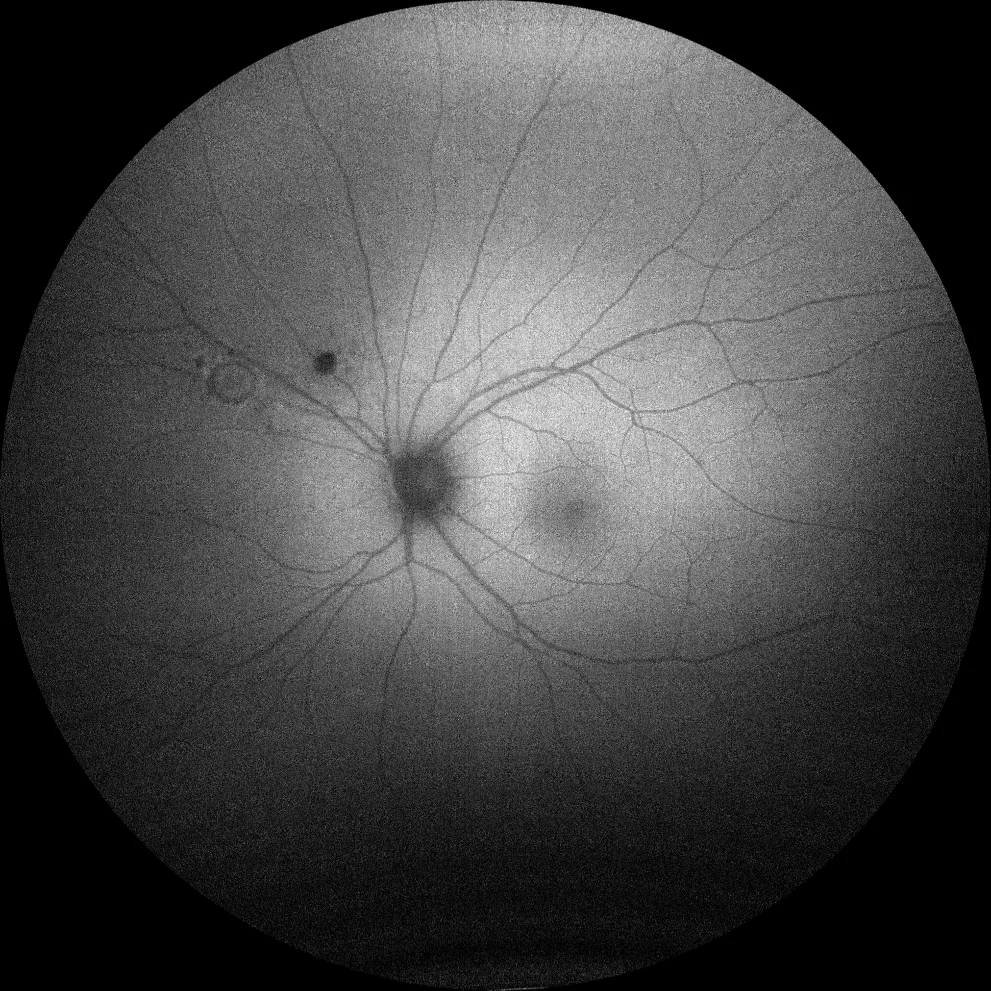
B. Autofluorescence (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye hypoautofluorescence in the old scar. The active lesion shows a more hypoautofluorescent center due to retinal opacity, with a hyperautofluorescent halo indicating activity.
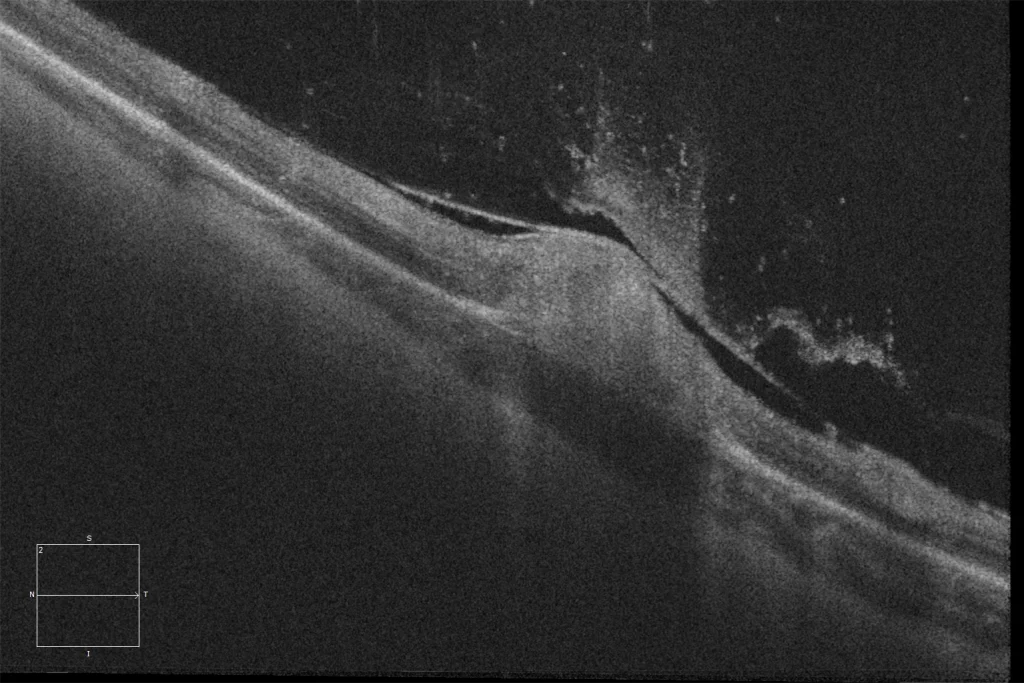
C. Optical coherence tomography (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) over the active lesion showing thickening with hyperintensity of the retina and disruption of the inner retinal layers (DRIL), as well as thickening of the posterior hyaloid and cellularity in the vitreous (vitreous hyperintense spots).
Description
Toxoplasmosis is the most common cause of infectious chorioretinitis in humans. It is caused by Toxoplasma gondii , an obligate intracellular parasitic protozoan whose definitive host is the cat and other felines. Infection rates are higher in tropical areas. This infection causes necrotizing retinitis with vasculitis, with the typical image being a “beacon in the fog,” representing the white focus of retinitis beneath vitreous inflammation. It may be classically accompanied by an adjacent pigmented scar corresponding to an old flare, as well as vasculitis (Kyrieleis arteriolitis is typical), ocular hypertension, or other signs of granulomatous inflammation. Recurrence usually occurs at or near the margins of the old lesion, and the risk is highest in the first year after the flare and in older individuals. The classic treatment is triple therapy with pyrimethamine, sulfadiazine, and systemic corticosteroids, along with folinic acid supplementation. In Spain, high-dose cotrimoxazole is an acceptable alternative.