Retinal vasculitis associated with tuberculosis
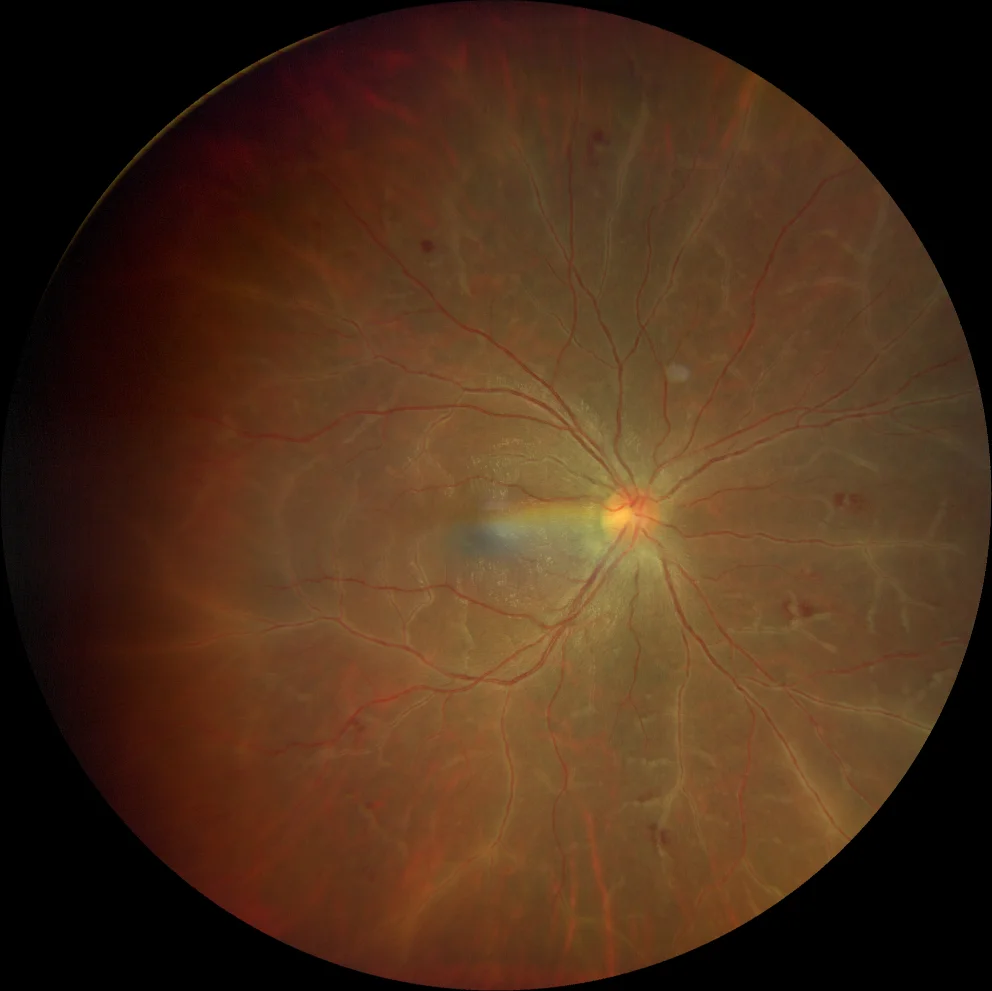
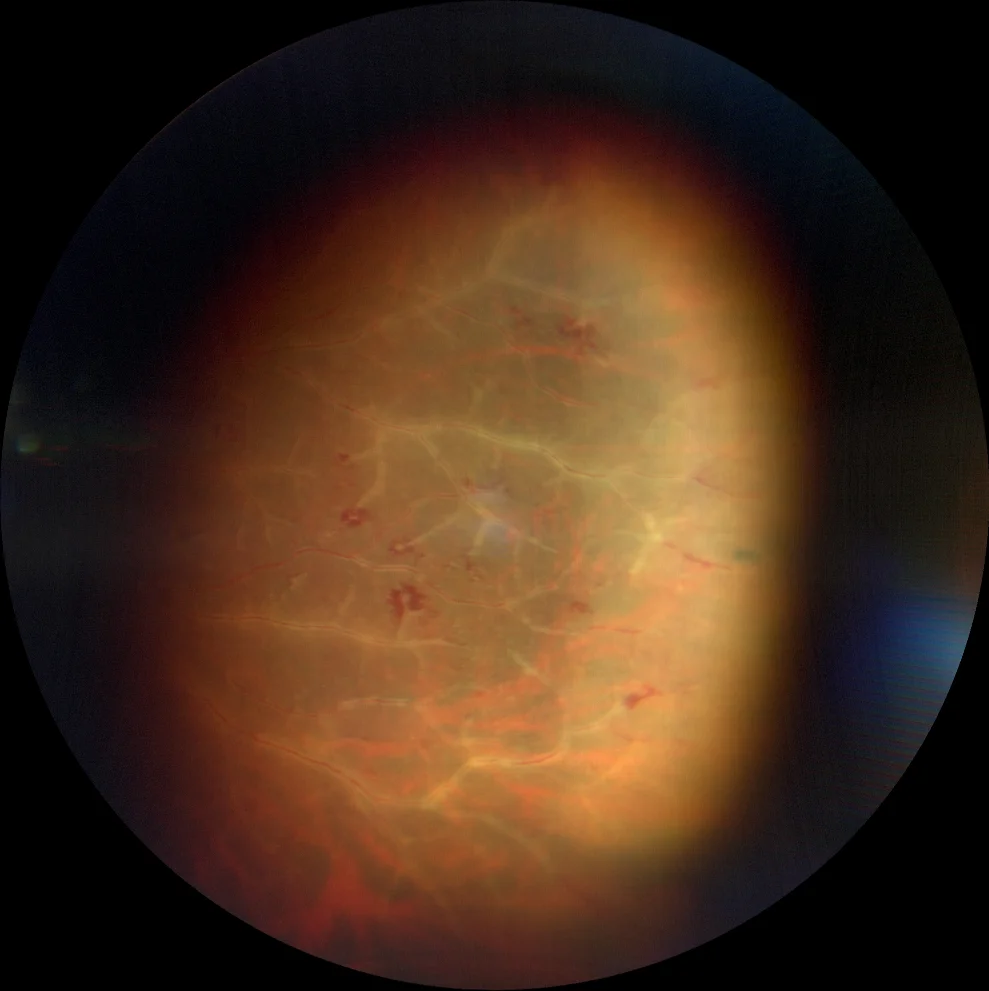
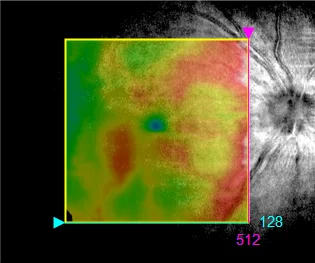
A and B. Color fundus photographs (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right eye showing diffuse periphlebitis and spot hemorrhages in the periphery.
A and B. Color fundus photographs (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right eye showing diffuse periphlebitis and spot hemorrhages in the periphery.
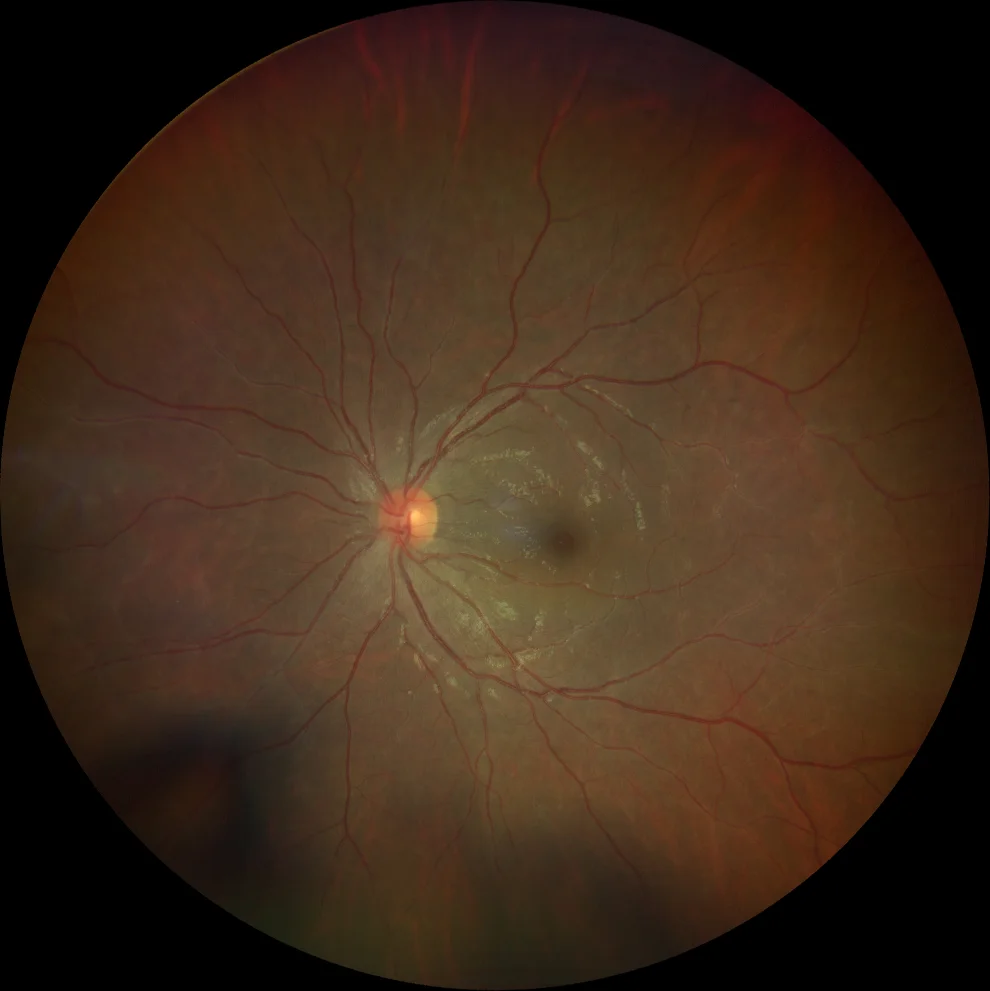
C. Color retinography (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye showing periphlebitis in the nasal vessels
Description
Retinal vasculitis associated with tuberculosis is a heterogeneous and difficult to manage entity. It is characterized by occlusive retinal vasculitis, predominantly venous, with associated vitritis and peripheral retinal ischemia in patients with evidence of tuberculosis by laboratory test or biopsy. It typically appears as peripheral periphlebitis with a tendency to capillary closure and neovascularization. The lack of consensus in the diagnosis and management of this entity can lead to sequelae. Treatment is based on the use of antituberculosis drugs accompanied or not by oral steroid treatment and even immunosuppressants. Treatment success is defined as the resolution of inflammatory signs 6 months after finishing treatment, the ability to reduce the dose of oral steroids below 10 mg/day or 1 drop of oral steroids maximum every 12 hours. Sometimes, local complications such as neovascularization or tractional retinal detachment require additional treatment.