Macular serpiginous choroiditis
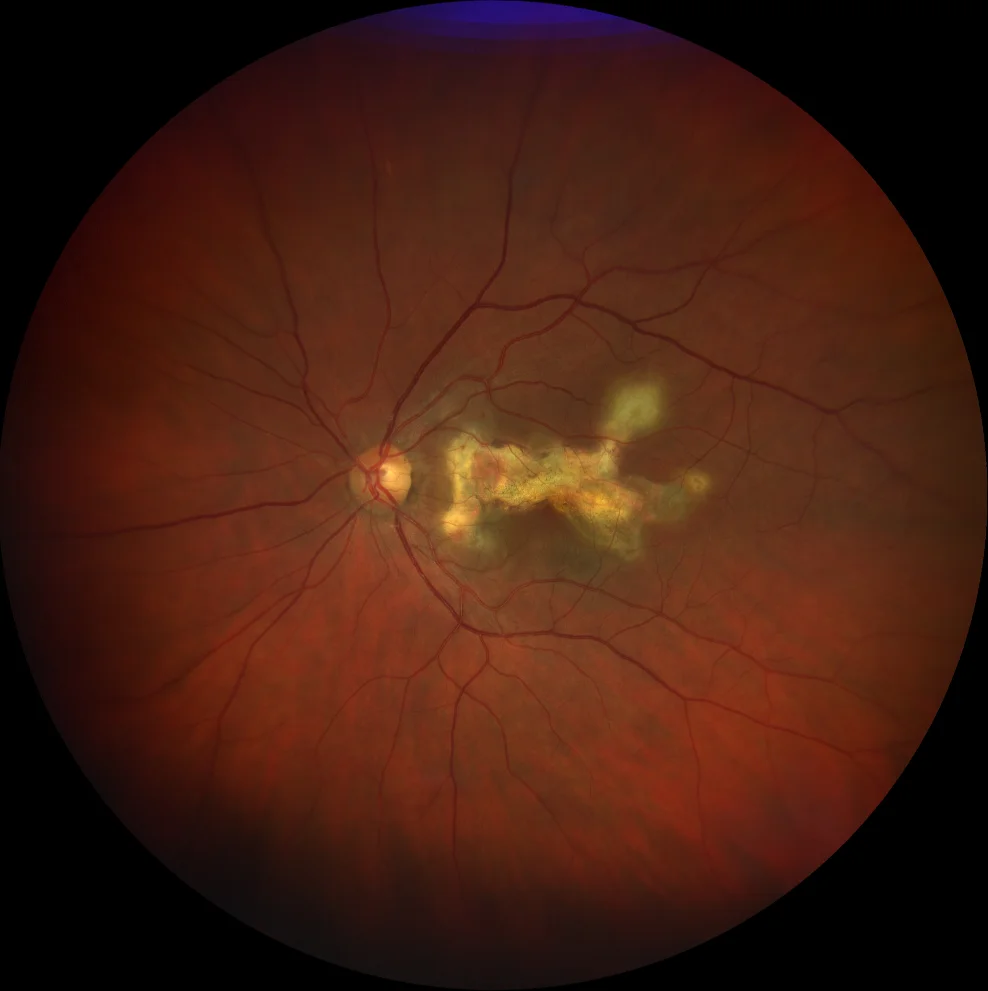
A. Color fundus image (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye showing a macular lesion with irregular borders, more atrophic areas in the center and creamier edges (active choroiditis).
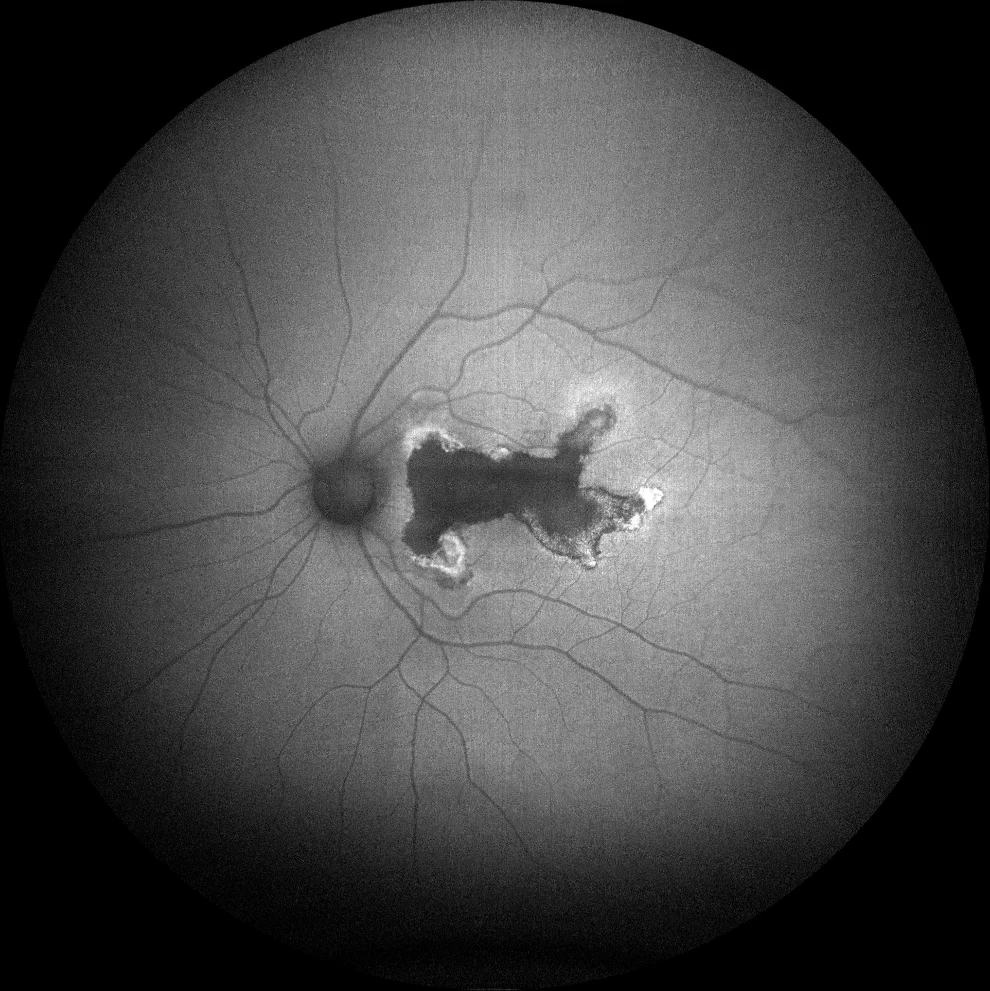
B. Autofluorescence (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye showing hypoautofluorescence in the central atrophic areas and hyperautofluorescent rims corresponding to areas of active choroiditis.
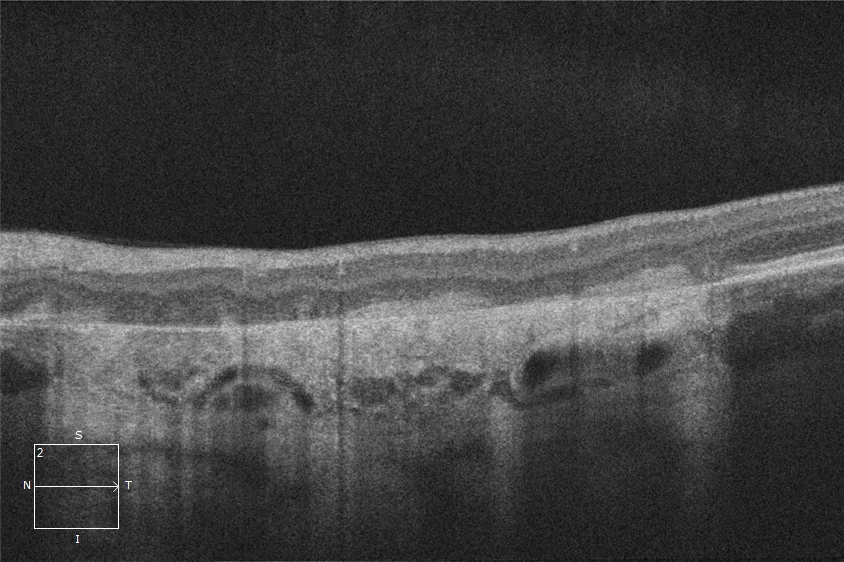
C. Optical coherence tomography (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) over the lesion, showing loss of the ellipsoid layer in the lesion area, together with accumulations of subretinal hyperreflective material, which corresponds to the areas of fibrosis.
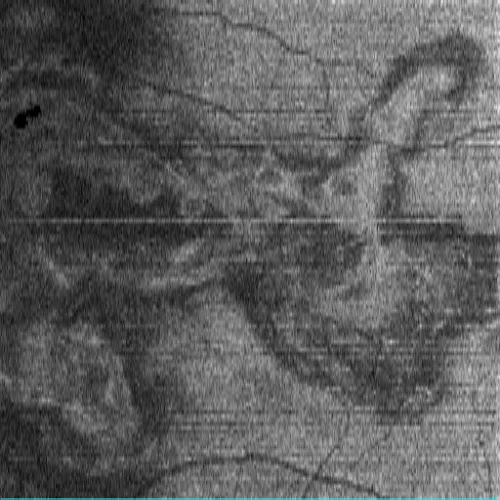
D. En face image of macular optical coherence tomography (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye at the level of the ellipsoid, loss of the external segments of the photoreceptors in the area of the lesion.
Description
Serpiginous choroiditis is an inflammation of the choriocapillaris and retinal pigment epithelium (RPE) of unknown etiology, although an autoimmune origin with probable vascular occlusion at the level of the choriocapillaris is suspected. In active lesions, poorly defined creamy borders can be observed in the fundus, possibly showing edema of deep layers of the retina, with the lesions evolving towards chorioretinal atrophy with a typical serpiginous form. In active phases, autofluorescence shows hyperautofluorescent halos surrounding hypoautofluorescent lesions. In chronic lesions, complete hypoautofluorescence with sharp borders is observed. In optical coherence tomography, areas with disruption of the outer layers of the retina and edema coexist with inactive areas of atrophy and fibrosis. It is very important, due to its therapeutic implications, to assess whether there is peripapillary involvement and vitritis. In cases where serpiginous choroiditis is suspected but the peripapillary area is spared, serpiginous-like choroiditis should be suspected. In this clinical case, the IGRA results were negative. Therefore, immunosuppressive treatment was started with a good response.