Macular telangiectasias type 2
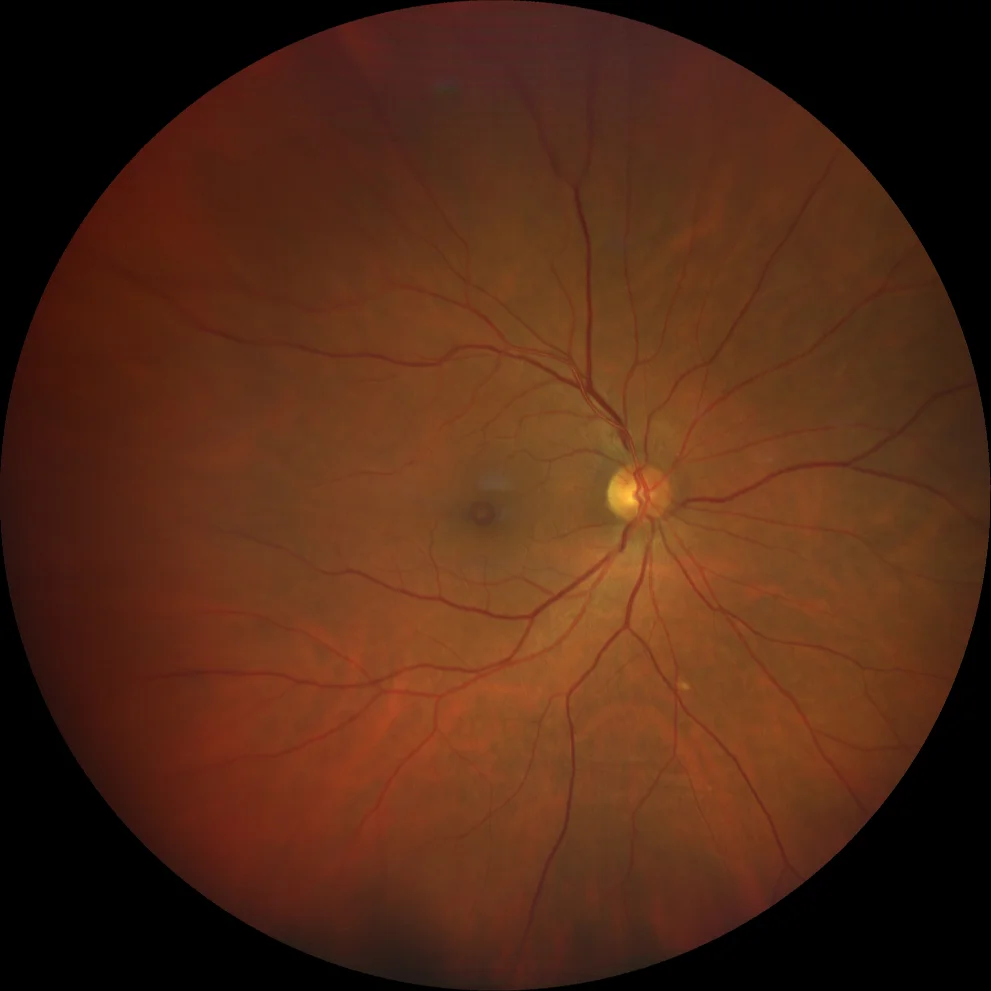
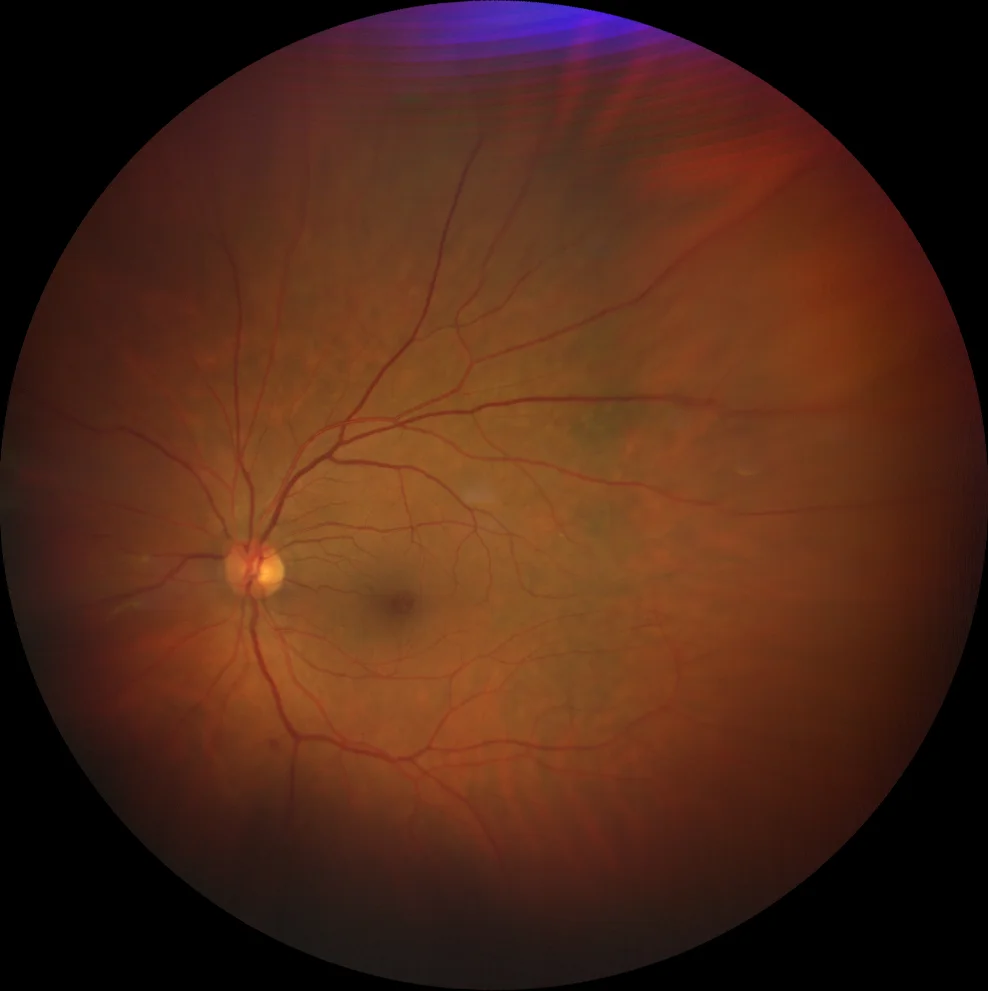
Macular telangiectasias type 2. A and B. Color fundusography (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing a bilateral lamellar hole image.
Macular telangiectasias type 2. A and B. Color fundusography (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing a bilateral lamellar hole image.
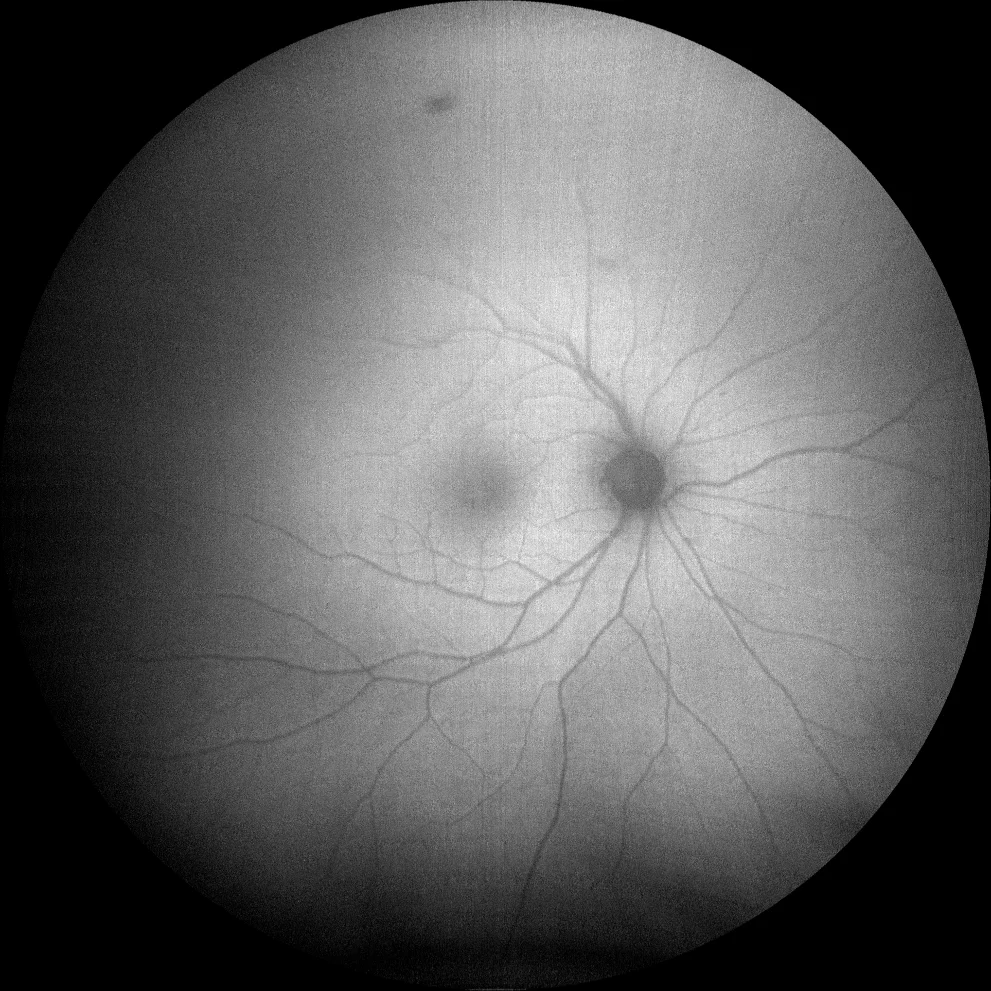
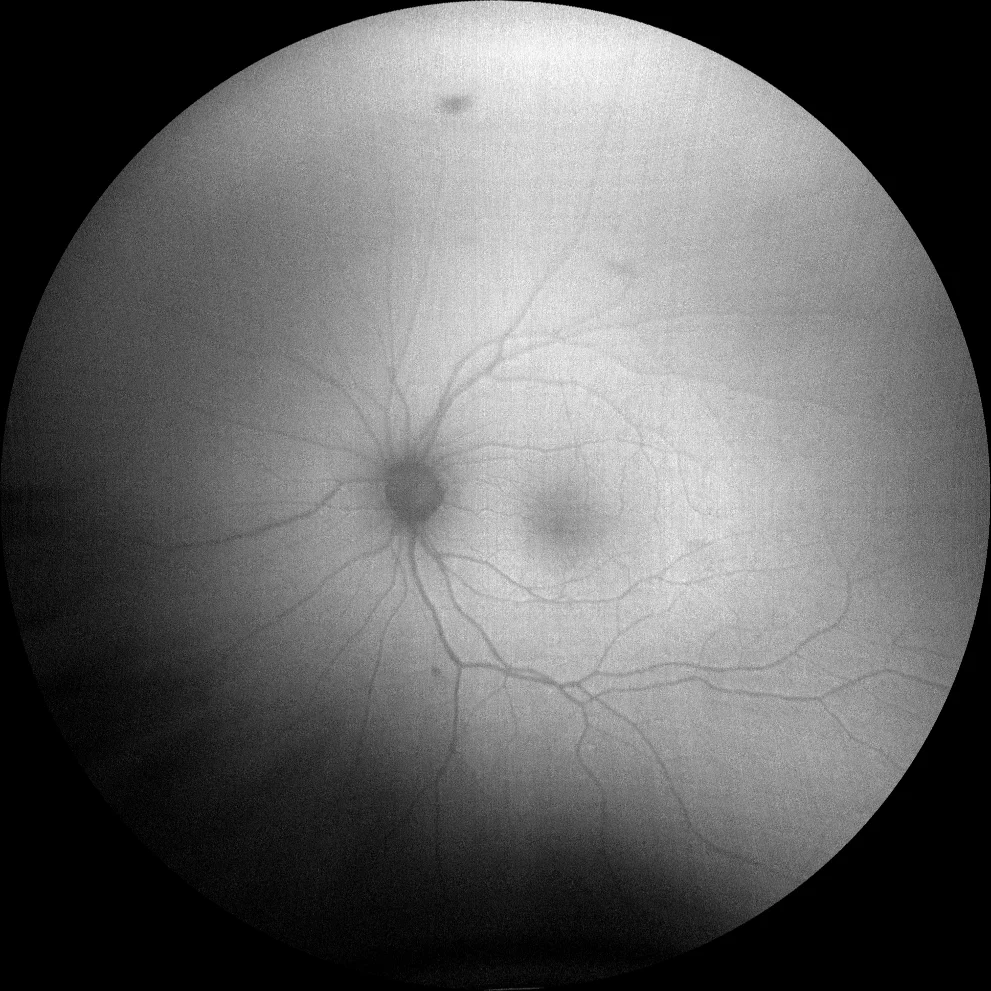
C and D. Autofluorescence images (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing mild hyperautofluorescence temporal to the fovea.
C and D. Autofluorescence images (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing mild hyperautofluorescence temporal to the fovea.
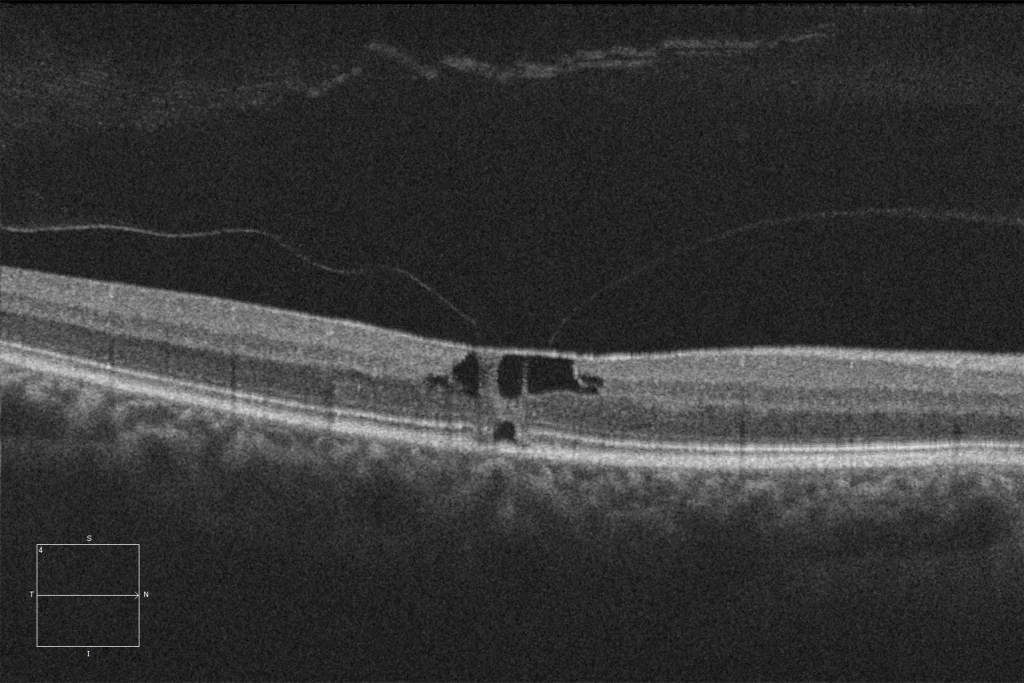
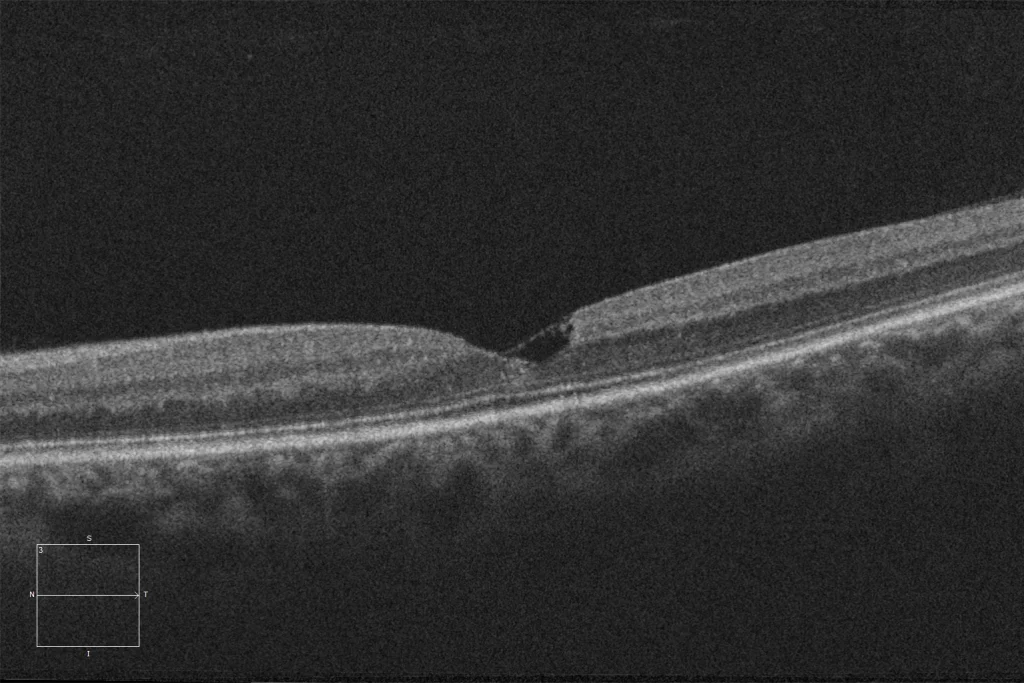
E and F. Macular HD optical coherence tomography (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes showing bilateral inner retinal defects with preservation of the internal limiting membrane (ILM draping). In the right eye, there is also an outer retinal defect with loss of the ellipsoid layer at the subfoveal level.
E and F. Macular HD optical coherence tomography (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes showing bilateral inner retinal defects with preservation of the internal limiting membrane (ILM draping). In the right eye, there is also an outer retinal defect with loss of the ellipsoid layer at the subfoveal level.
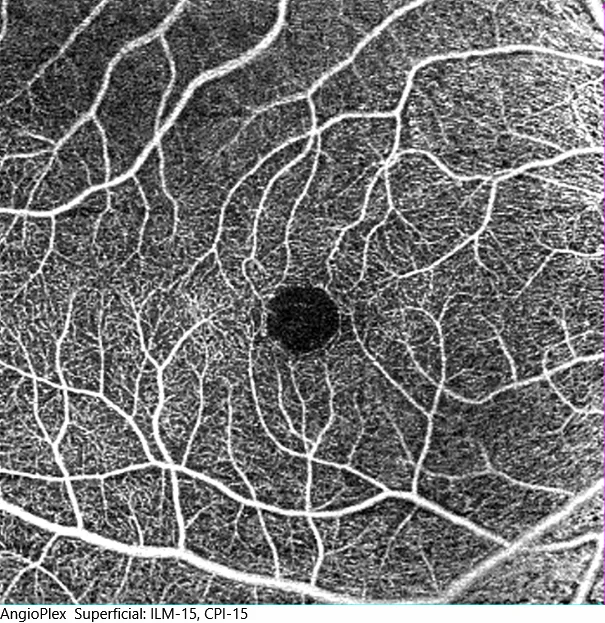
G and H: Optical coherence tomography angiography at the level of the superficial macular plexus (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing an increase in the size of the foveal avascular zone (FAZ), together with remodeling of the vascularization of the temporal border of the FAZ. I: Optical coherence tomography angiography at the level of the deep macular plexus (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye, showing vessels at right angles temporally to the fovea, communicating the superficial and deep plexuses.
G and H: Optical coherence tomography angiography at the level of the superficial macular plexus (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the right and left eyes, showing an increase in the size of the foveal avascular zone (FAZ), together with remodeling of the vascularization of the temporal border of the FAZ. I: Optical coherence tomography angiography at the level of the deep macular plexus (Cirrus 5000, Carl Zeiss Meditec ASG, Jena, Germany) of the left eye, showing vessels at right angles temporally to the fovea, communicating the superficial and deep plexuses.
Description
Macular telangiectasias type 2 (MacTel 2) usually present bilaterally, asymmetrically and with slow progression. It is a neurodegenerative process of slow evolution. The findings in the ophthalmoscopic examination of the posterior pole are variable depending on the severity of the pathology. The earliest funduscopic alteration is usually a grayish coloration, usually of the temporal juxtafoveal retina, secondary to a loss of transparency of the same. Another characteristic finding of this pathology is the appearance of venular dilatations associated with a right-angle arrangement of said vascular structures. In addition, it is possible to find pigmentary alterations related to a hyperplasia of the retinal pigment epithelium, as well as crystalline deposits.
Regarding OCT, the most typical finding is hyporeflective spaces without associated retinal thickening, which may be accompanied by alterations in the underlying outer layers. The preservation of the internal boundary over the hyporeflective spaces (ILM draping) is characteristic. In cases of associated choroidal neovascularization, this will appear as a hyperreflective structure. Pigment deposits will also be visualized as structures with increased reflectivity. Regarding optical coherence tomography angiography (OCT-A), a decrease in vascular density may initially be observed, as well as telangiectatic vessels in the deep plexus of the temporal area, with the rest of the quadrants and the superficial plexus being affected as the pathology progresses. Using OCT-A, it is also possible to detect the presence of neovascular membranes.
Regarding the autofluorescence study, a common finding present in early stages of the disease is the increase in fluorescence in the macular area. Regarding fluorescein angiography, it is possible to observe vascular dilatations with leakage in early stages and diffuse hyperfluorescence in late stages.