Retinal pigment epithelium (RPE) tear
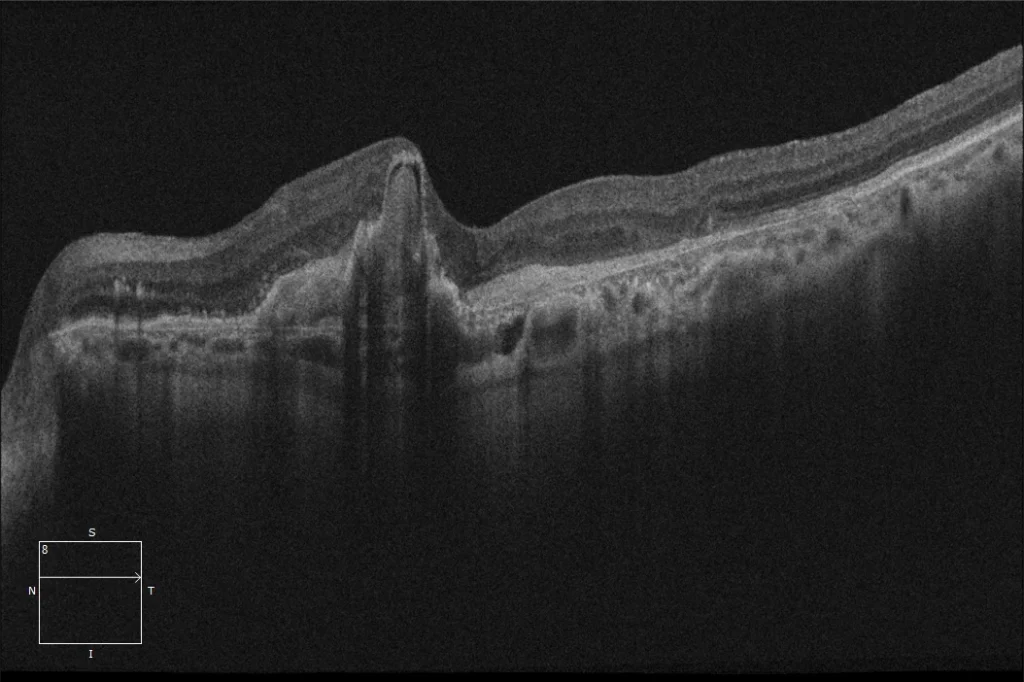
(A)OI: Neovascular AMD with RPE tear. It can be seen that the area temporal to the lesion, reaching the fovea, is composed of an area of denuded RPE (blacker in colour and showing choroidal vessels), where there is no RPE since, upon tearing, it has retracted towards the nasal area. In the nasal area of the lesion, the RPE is retracted and folded and is darker brown in colour. The traction of the neovascular membrane on one of the edges of the PED causes the RPE to tear and makes said RPE retract and fold towards the contralateral side.
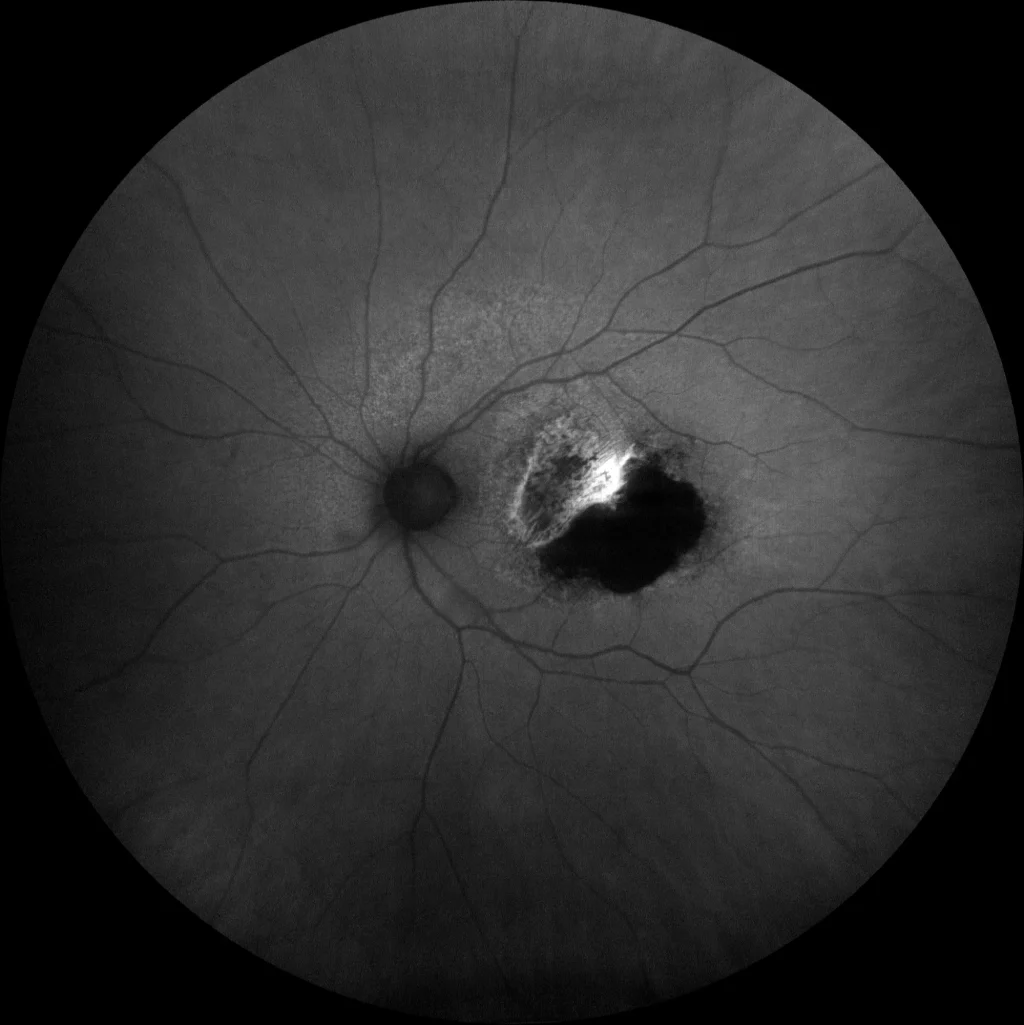
• Autofluorescence (Clarus500, Zeiss): (B) LE: Absolute hypoautofluorescence is observed in the area of denuded RPE (temporal area of the lesion) due to the absence of RPE cells in that area. Hyperautofluorescence appears on the nasal edge of the hypoautofluorescence, produced by an increase in RPE in that area as it is retracted and folded over itself.
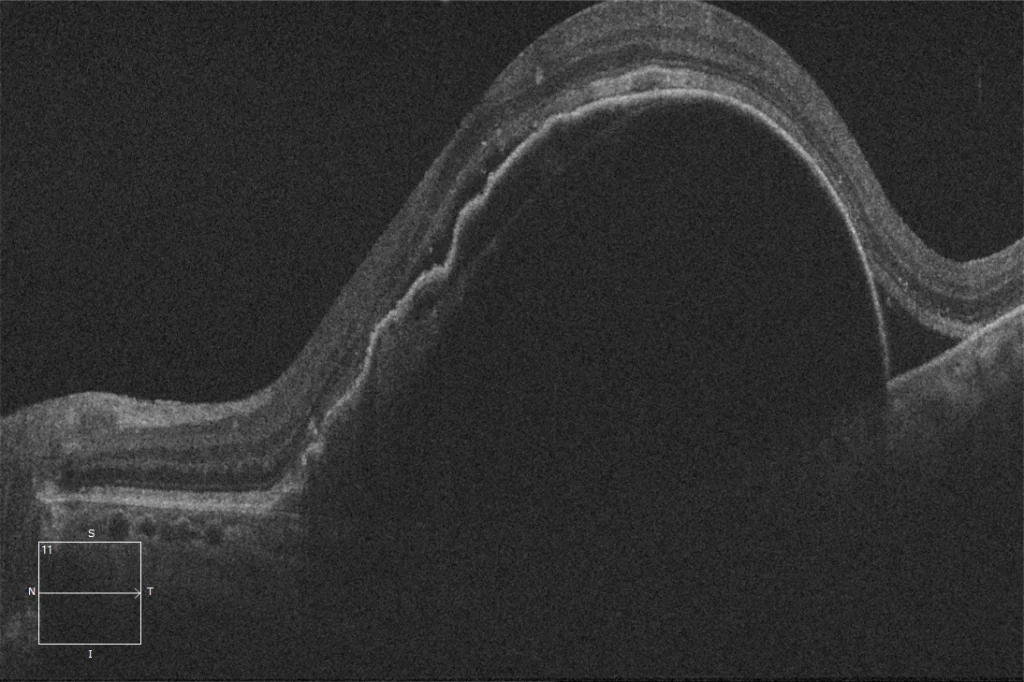
(C) OCT macular pre-RPE tear LE: PED with high-risk features (tall and wide, RPE ripples, arcuate Bruch's membrane) for RPE tear, and presence of subretinal fluid. A hyperreflective lesion can be seen adhered to the posterior surface of the RPE, which probably corresponds to the neovascular membrane.
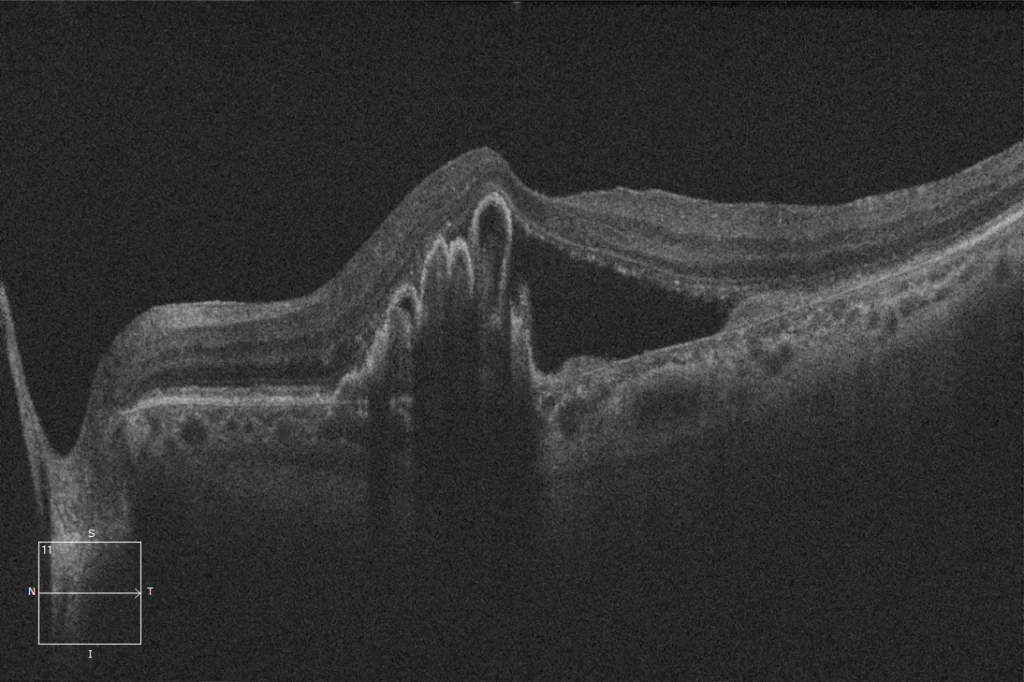
(D) Macular OCT after LE tear: The image shows an absence of RPE in the temporal sector of the lesion affecting the fovea, with said RPE completely retracted and folded in the nasal part.
Description
RPE tear is a disruption of the RPE monolayer that occurs in the context of pigmented epithelial detachment (PED) generally associated with the presence of a type 1 neovascular membrane. The main hypothesis is that the neovascular membrane would be adhered to the posterior face of the RPE under the PED and when contracting would pull on the RPE of one of the edges of the PED causing its rupture and retraction. Although it can occur spontaneously, treatment with antiangiogenics increases the risk by 17-21% by promoting said membrane contraction. Certain characteristics of the PEDs, including diameter greater than 5 mm, height> At 550 microns, undulations/irregularities of the RPE, buckling of the Bruch membrane in a suspension bridge or hyperfluorescent ring are considered risk factors for this pathology. When they occur, the recommended treatment is to continue with antiangiogenic treatment while there is neovascular activity.