Macular neovascularization type 3
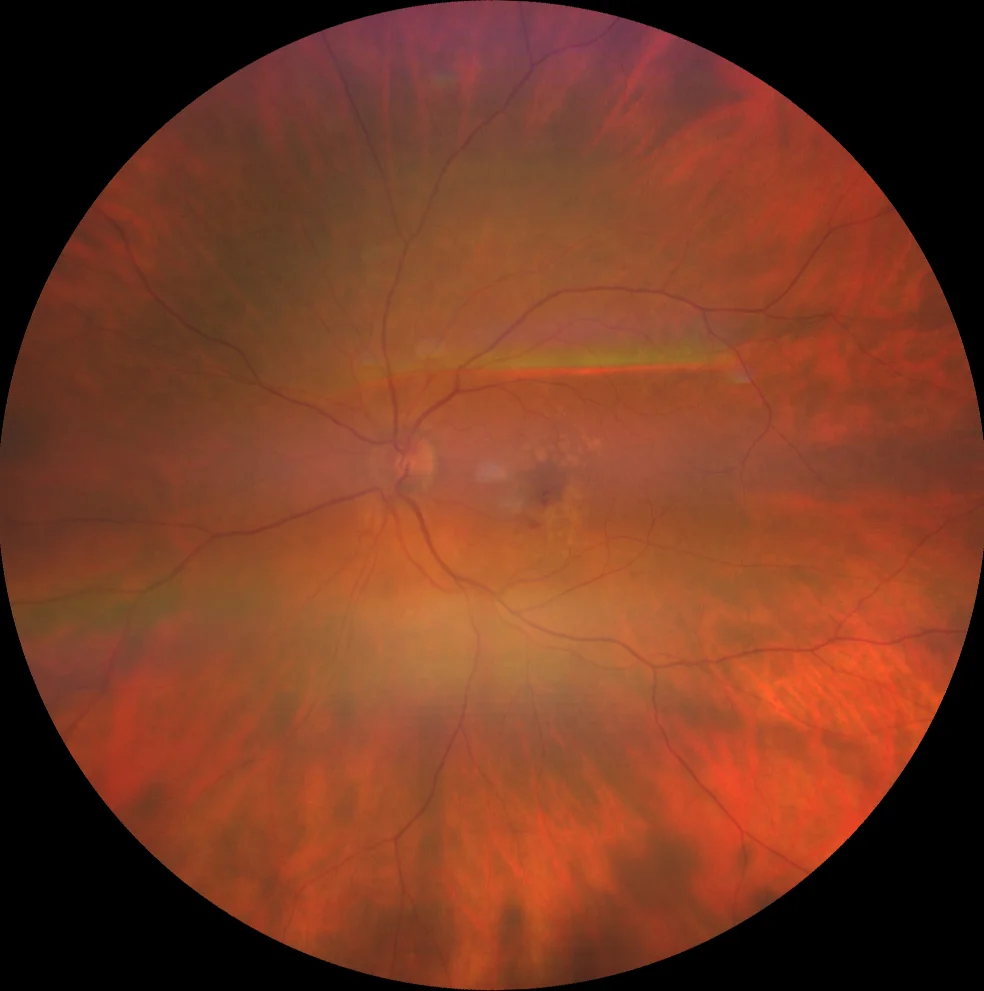
A: Two macular hemorrhages are observed, called sentinel hemorrhages because they indicate the location of the neovascular complex. Confluent soft drusen are also observed.
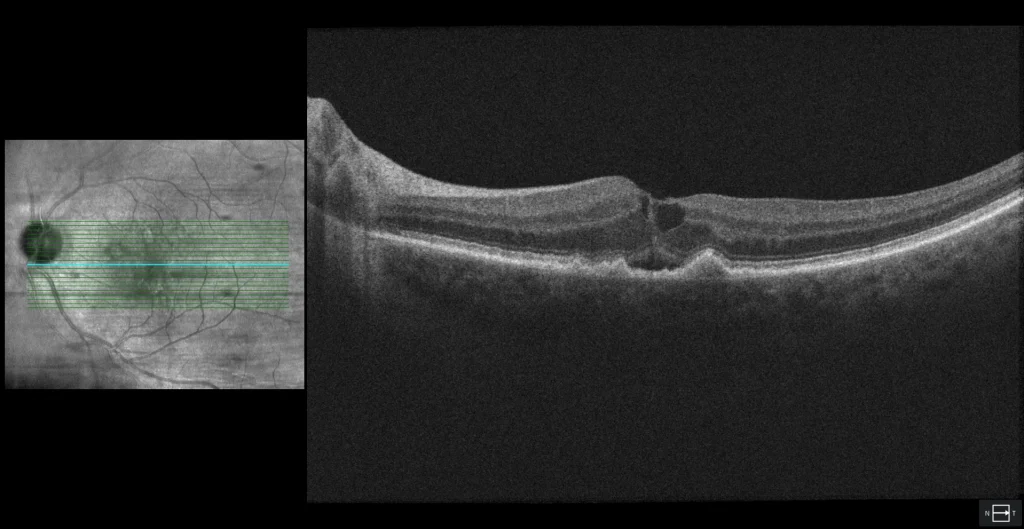
B1: Foveal cross section of the LE showing the elevations of the RPE corresponding to soft drusen, as well as intra- and subretinal fluid.
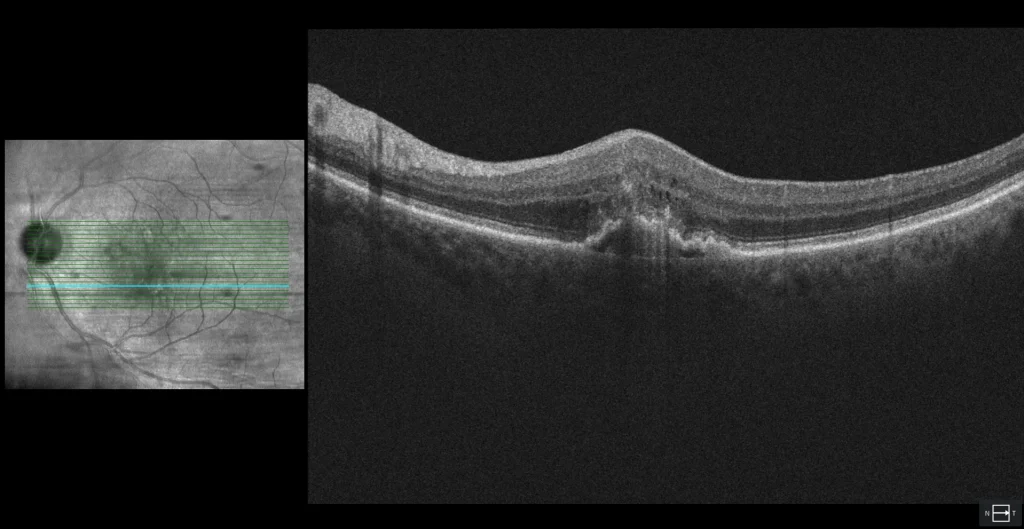
B2: cross section of the lower macula. A hyperreflective lesion is observed in the outer layers of the retina, over an irregular (fibrovascular) PED. The latter presents a rupture of the RPE, which is where the intraretinal and sub-RPE neovascular components communicate (retinochoroidal anastomosis). Small cysts of intraretinal fluid are also observed, which is very characteristic of type 3 NVM.
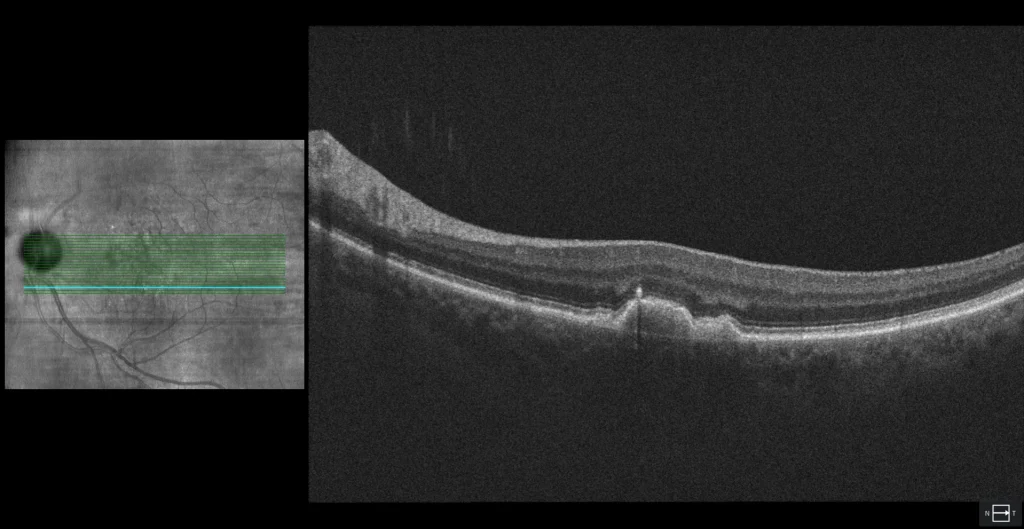
B3: cross section at the same location as B2, but taken 6 months earlier. A PED with an overlying hyperreflective spot can be seen separating from the RPE. The etiopathogenic hypothesis of type 3 NVM suggests that RPE cells in a PED are in hypoxic conditions. For this reason, they synthesize proangiogenic molecules such as VEGF. These cells separate from the rest of the RPE and migrate towards the inner retina. When they encounter the vascular endothelium of the deep retinal plexus, this excess of VEGF leads to the formation of an intraretinal neovascular complex.
Description
76-year-old woman who comes due to loss of vision in her left eye.
VA in the RE is 20/20 and in the LE 20/50. She is pseudophakic in both eyes.
The patient presented neovascular AMD with type 3 NVM, so antiangiogenic treatment was started.