Anterior ischemic optic neuropathy – Non-arteritic
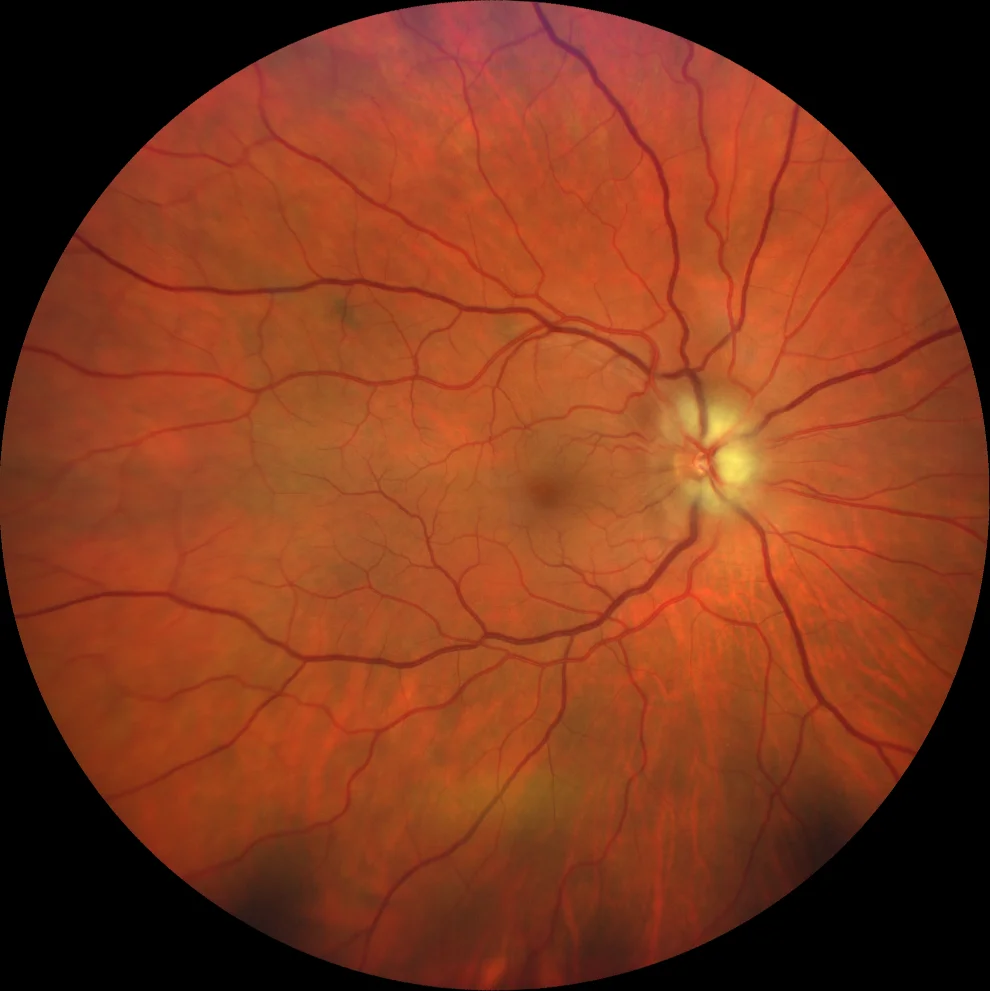
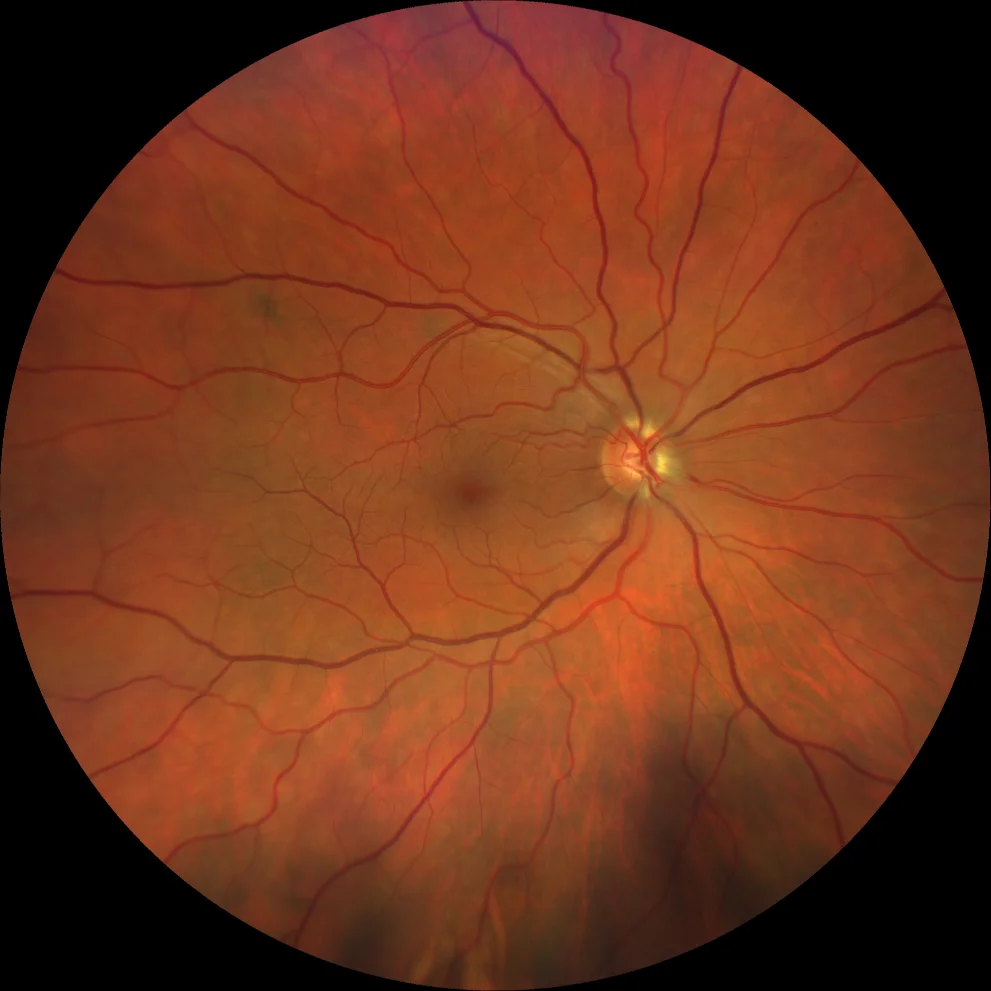
Retinography (Clarus 700, Zeiss): papilledema, with raised papilla and blurred edges (A1). After 1 week, the papilledema persists and 2 splinter hemorrhages appear (A2). After 3 weeks, the edema has almost completely resolved (A3).
Description
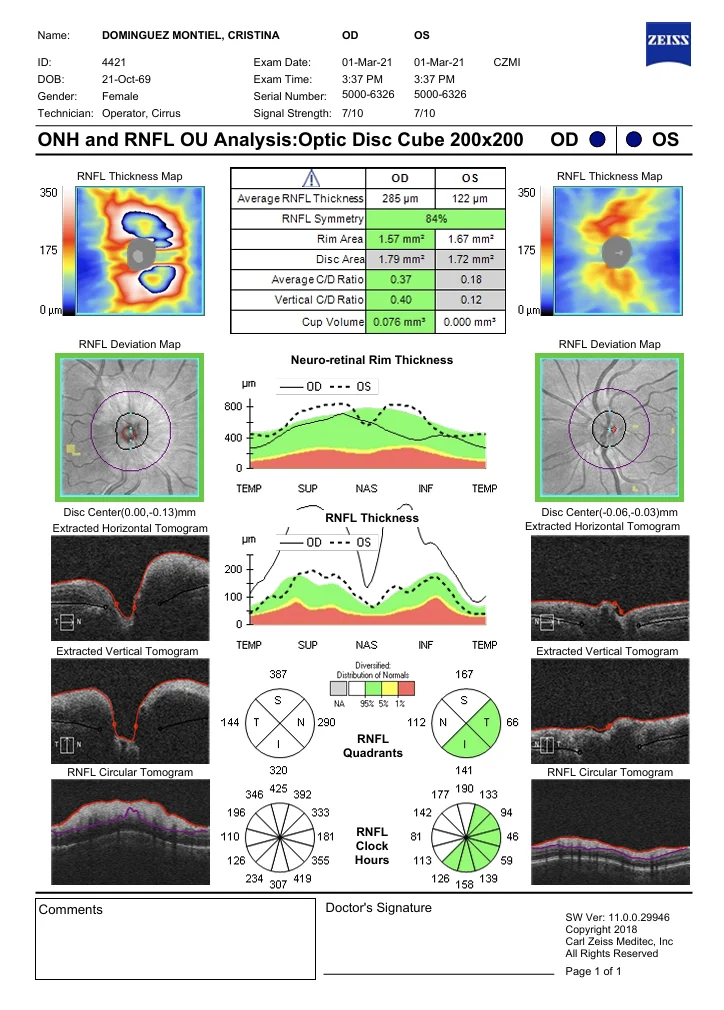
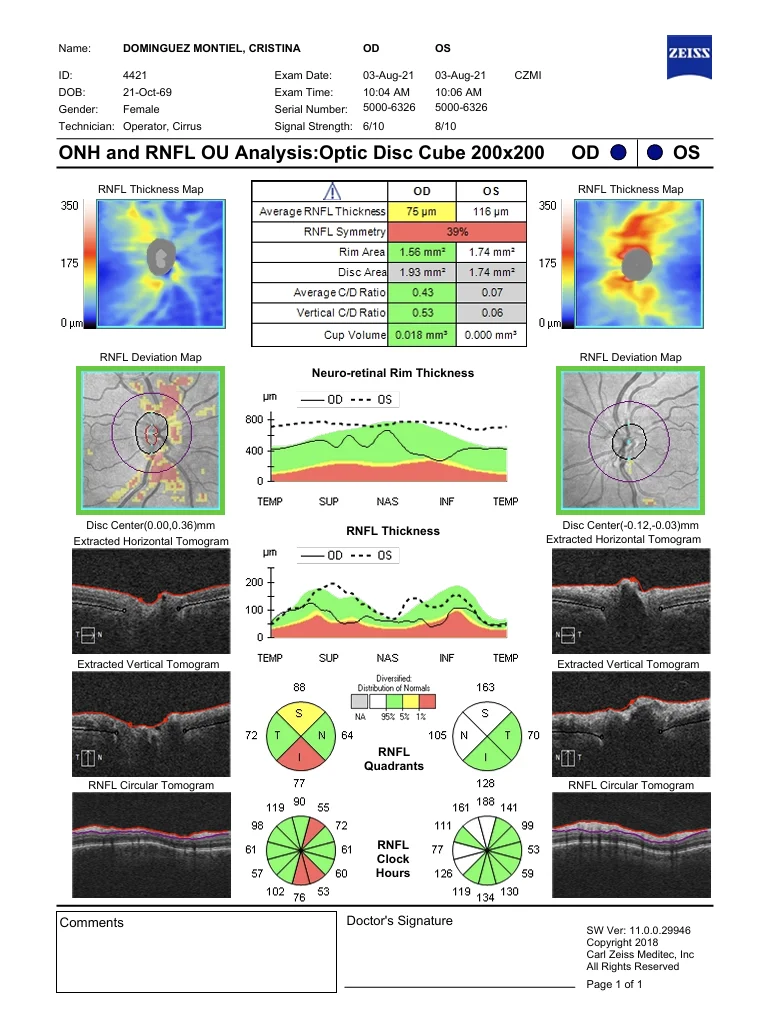
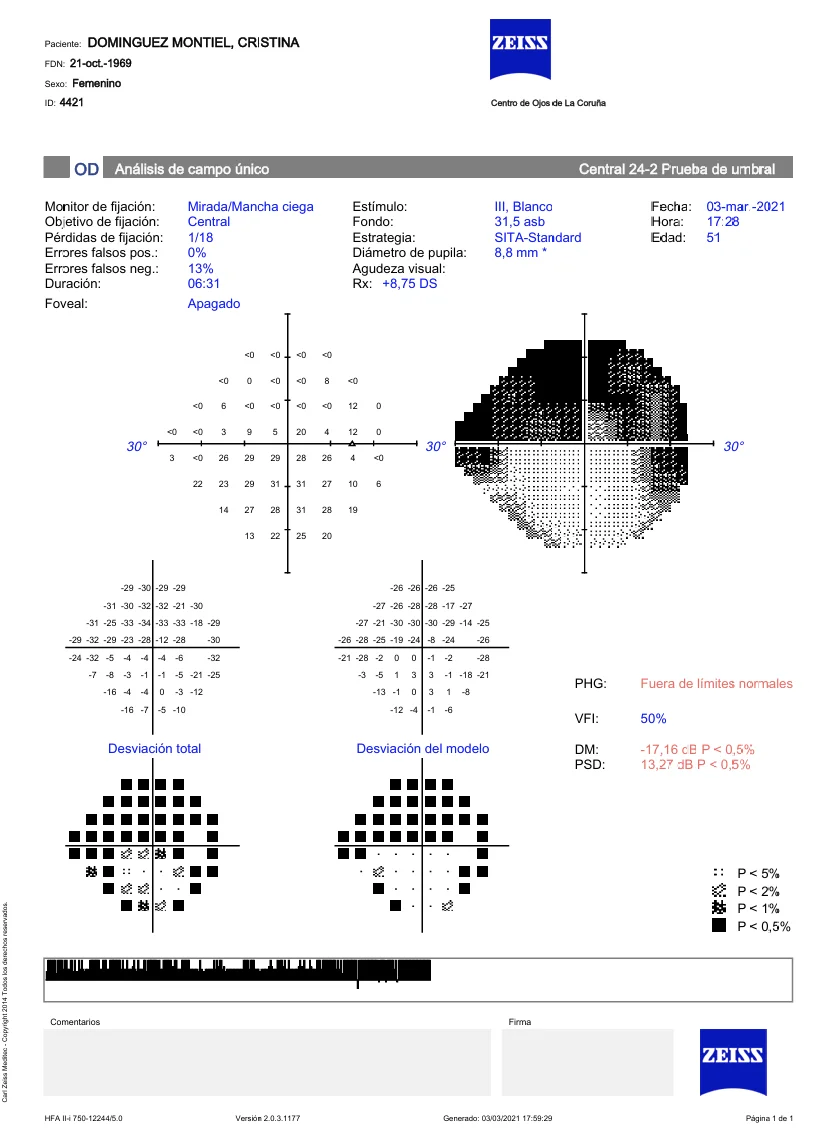
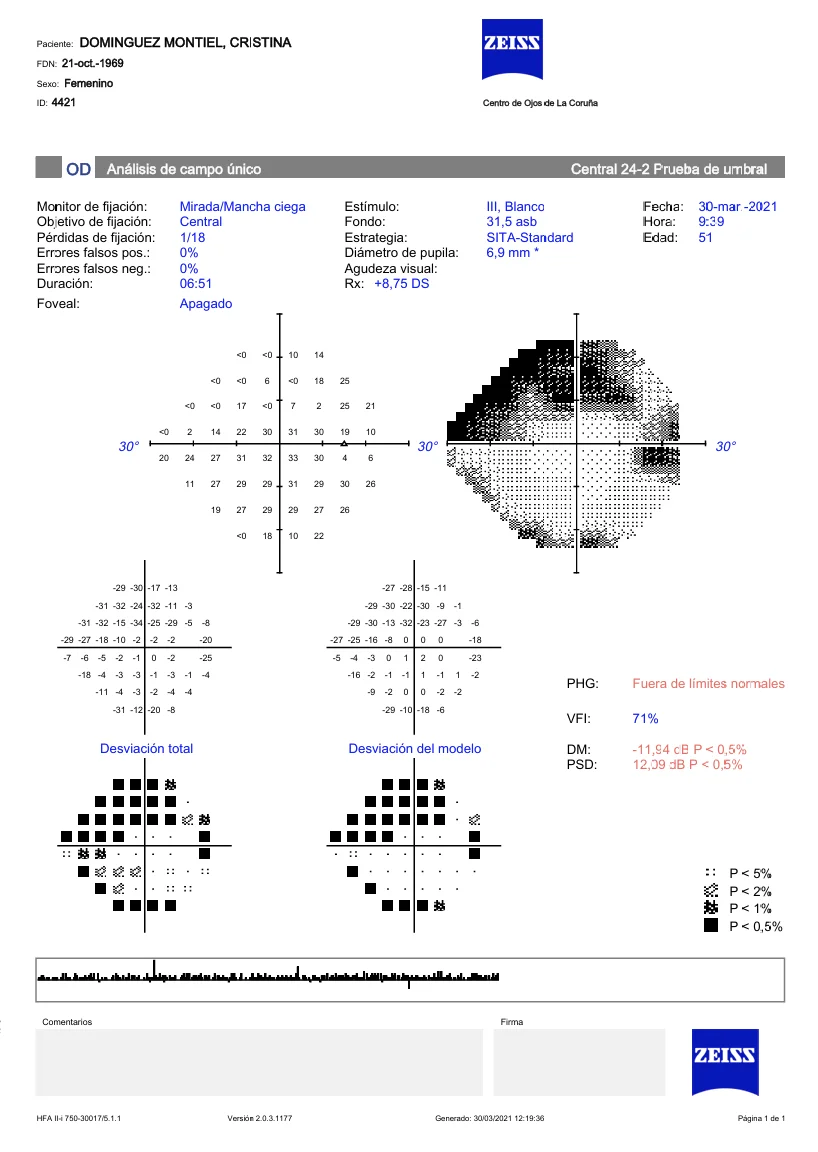
A 53-year-old woman, hyperopic (spherical equivalent OD +7.00 OI +6.50), complained of pain and red eye in the right eye that had been developing for 24 hours, 2 days after attending a check-up in which her pupils were dilated. Ciliary injection, stromal corneal edema, slightly reactive median mydriasis and OT of 45 mmHg were observed. After treatment with peripheral iridotomy with YAG laser and oral and topical hypotensive medication, OT dropped to 8 mmHg but the patient reported losing vision. VA was 20/20. The fundus showed an elevated papilla with blurred edges and edema. A severe increase in the fiber layer was observed in the OCT and campimetry revealed an upper altitudinal scotoma. The case was classified as non-arteritic anterior ischemic optic neuropathy (NAION). During follow-up, a progression towards atrophy in the OCT fiber layer and an improvement of the scotoma in campimetry was observed, although it was not completely resolved.