Central serous chorioretinopathy (CSC)
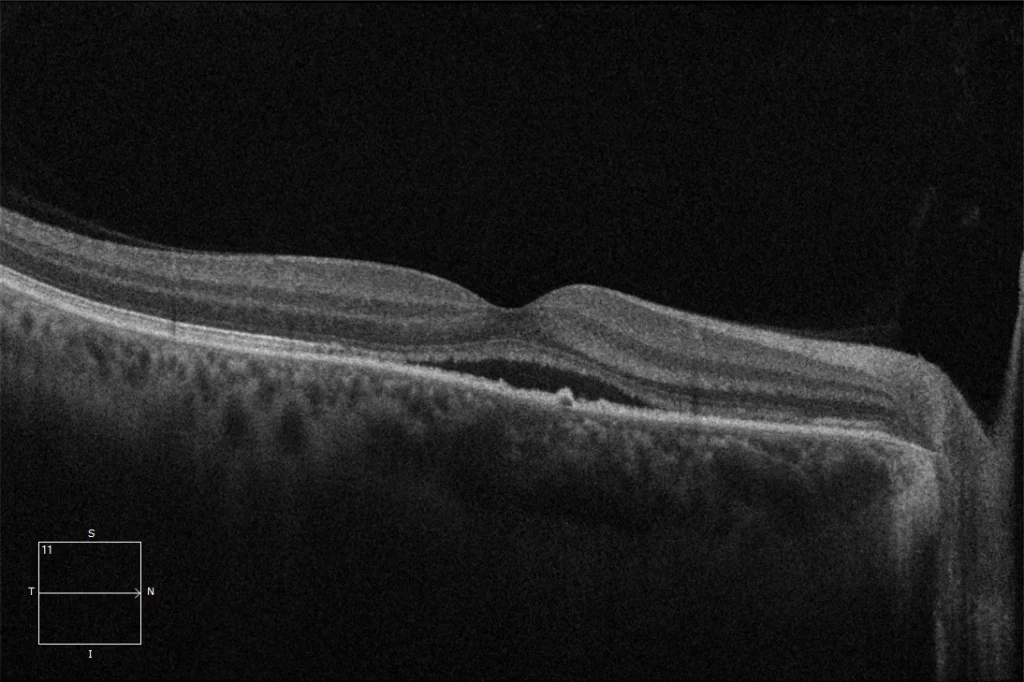
(A) Macular OCT 6 months pre-PDT OD: Acute phase of recurrence with the presence of hyporeflective subretinal fluid (SRF). A choroid with pachychoroid characteristics can be seen, thickened in the area nasal to the fovea. We can also observe a small irregularity in the retinal pigment epithelium. Section 2, taken in the area below the fovea, shows a retinal pigment epithelium detachment (RPE) that corresponds to the leak point.
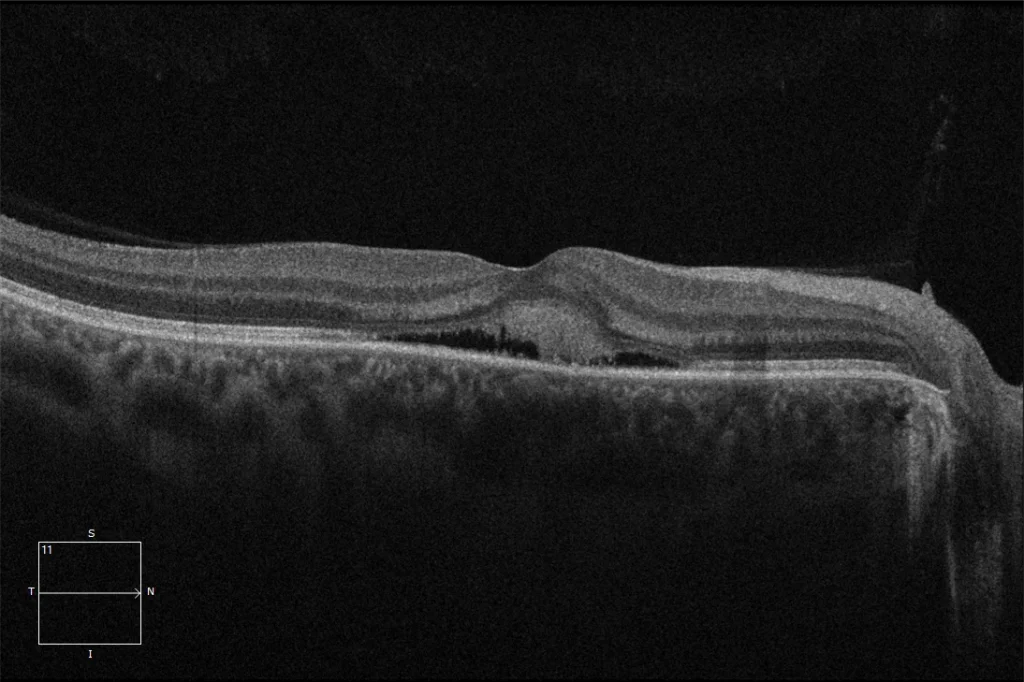
(B) Macular OCT 1 month pre-PDT OD: OCT shows FSR associated with hyperreflective material that usually represents fibrinoid material and is associated with chronicity and worse functional prognosis. Elongation of the outer segments of the photoreceptors is also evident.
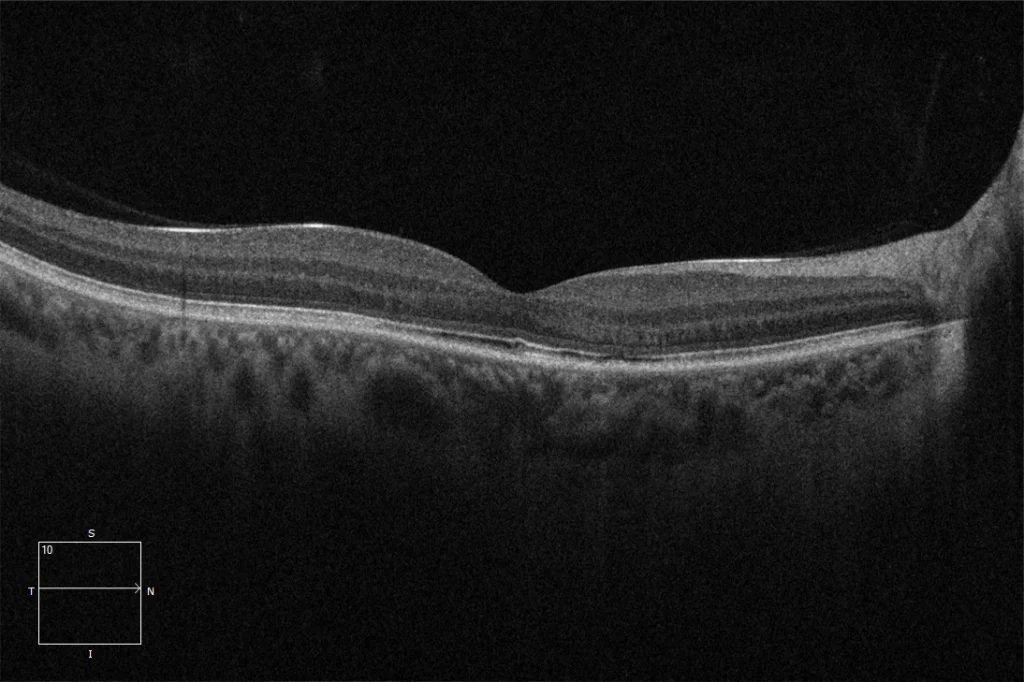
(C) Macular OCT 2 months post OD PDT: Resorption of the RBF, with some minimal irregularity of the RPE (despite the poor prognosis, the patient recovered unity of vision after low-fluence PDT)
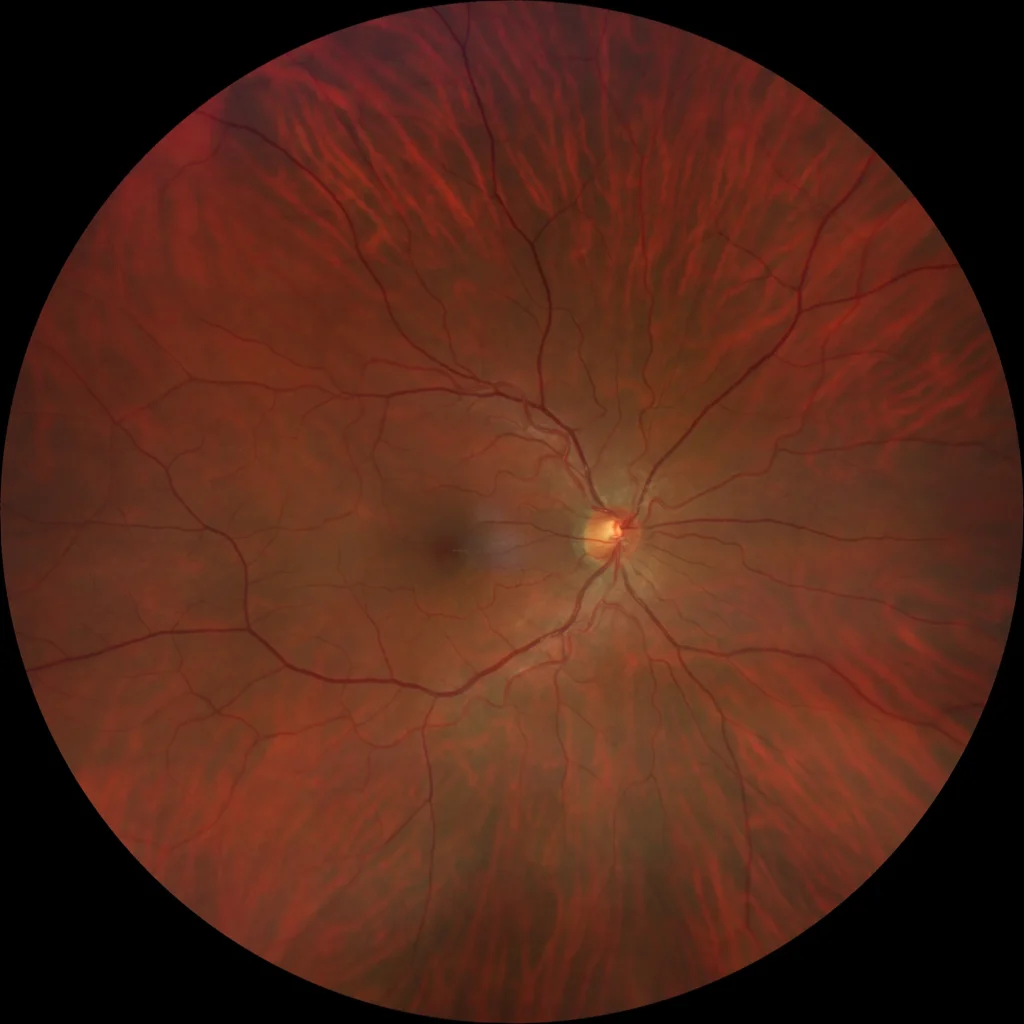
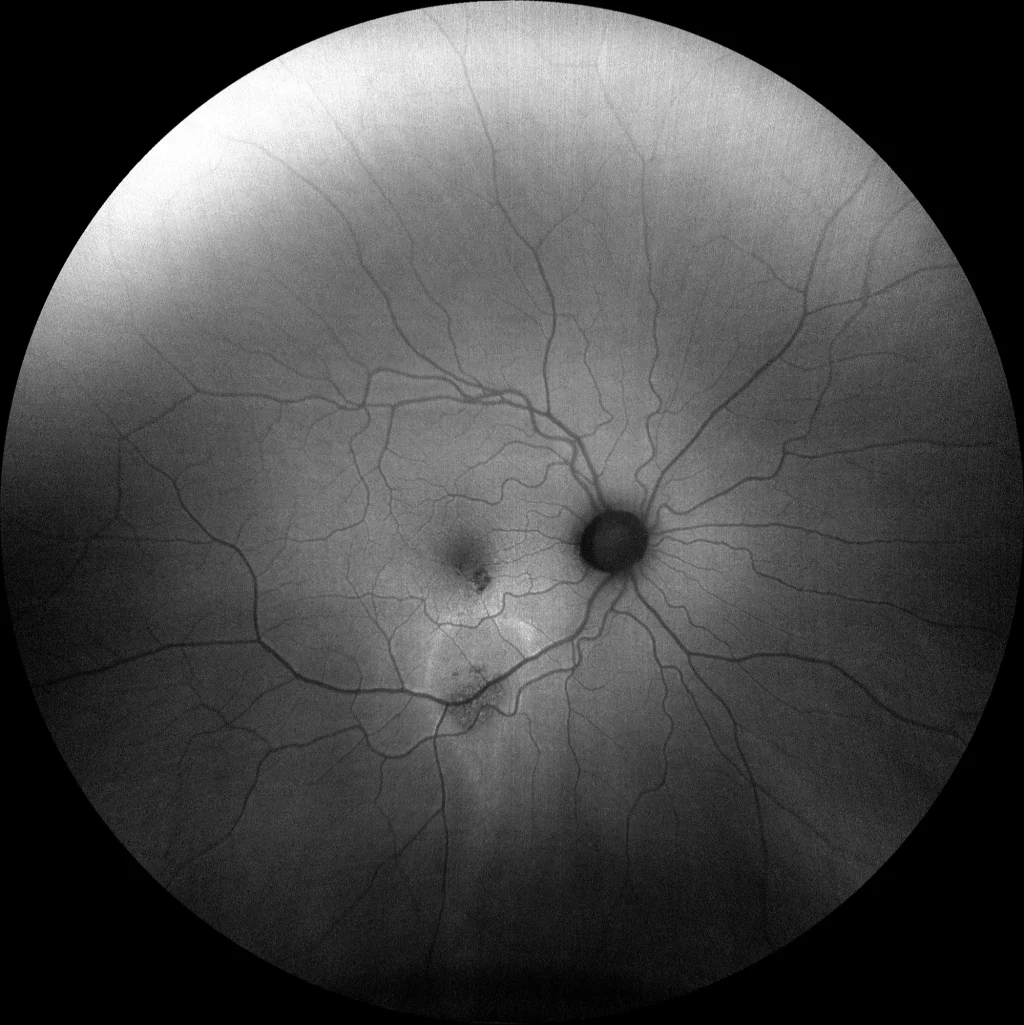
(D) OD: Minimal macular pigmentary alteration. Retinography does not show obvious alterations in the RPE. In these cases, autofluorescence may reveal sequelae of previous episodes of activity by highlighting alterations in the RPE in areas where fluid has accumulated.
(E) OD: Inferior juxtafoveal hypoautofluorescent lesion that appears to correspond to the vanishing point (VSP). Inferior to the macula, a "trail-like" hyperautofluorescent pattern is observed with a descending (gravitational) tract with greater hyperaurofluorescence at the edges, with an area of granular hypo-hyperautofluorescence within. The more marked hyperautofluorescence at the edges has been associated with the accumulation of precipitates and external segments of photoreceptors and the hypoautofluorescent areas with areas of RPE atrophy.
Description
Central serous chorioretinopathy (CSC). CSC is a pathology that is included within pachychoroid diseases. It is more frequent in men between 20-50 years of age, it is usually bilateral asymmetrical, and its exact causal mechanism is not fully established. However, it has been associated with steroids, both endogenous and exogenous, with type A personality, stress, the presence of Helicobacter Pilori infection and obstructive sleep apnea among others. Regarding the pathogenetic mechanism, it has been postulated that there is an increase in vascular permeability and choroidal hydrostatic pressure that could generate a dysfunction of the RPE that would lead to the accumulation of fluid in the subretinal space. The acute phase, therefore, usually occurs with the accumulation of subretinal fluid (neurosensory detachment) and sometimes, detachment of the pigmented epithelium that will generate a visual decrease and metamorphopsia. However, the acute phase is usually a self-limiting condition, with reabsorption of the subretinal fluid and recovery of vision in most patients within the first 3-6 months. However, between 30-50% of patients may experience recurrences within the first year and in up to 15-20% of cases the fluid and symptoms may persist beyond 6 months and are diagnosed with chronic CSC. When the condition becomes chronic or multiple recurrences occur, damage to the RPE cells and photoreceptors may occur, leading to irreversible visual impairment, or even the development of secondary neovascular membranes. Treatment of the acute phase is observation, since most resolve spontaneously. When fluid persists, various treatments have been published with different results, including laser photocoagulation, photodynamic therapy (PDT), antiangiogenics, mineralocorticoid antagonists, etc.