Coats disease
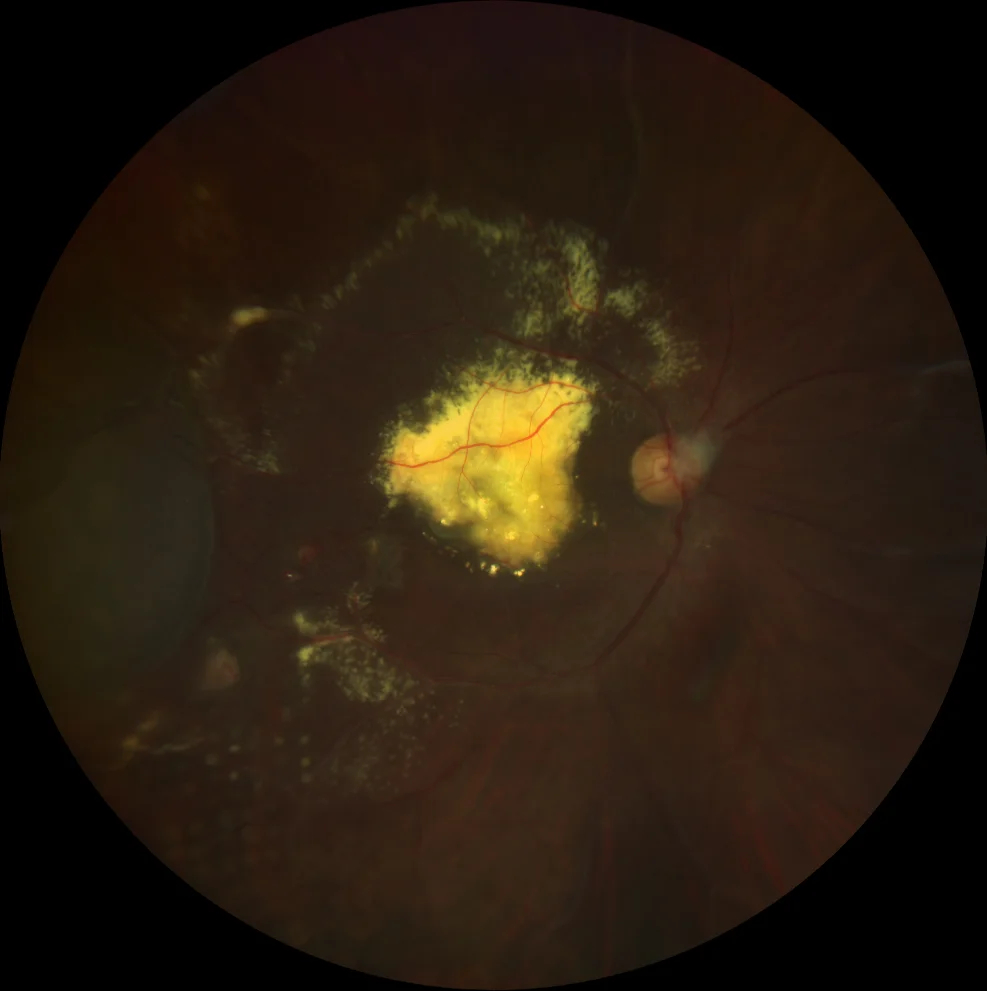
A. Color retinography (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the RE showing abundant macular lipid exudation extending beyond the vascular arcades, as well as a localized temporal exudative retinal detachment and sectoral panphotocoagulation scars in the temporal and lower periphery.
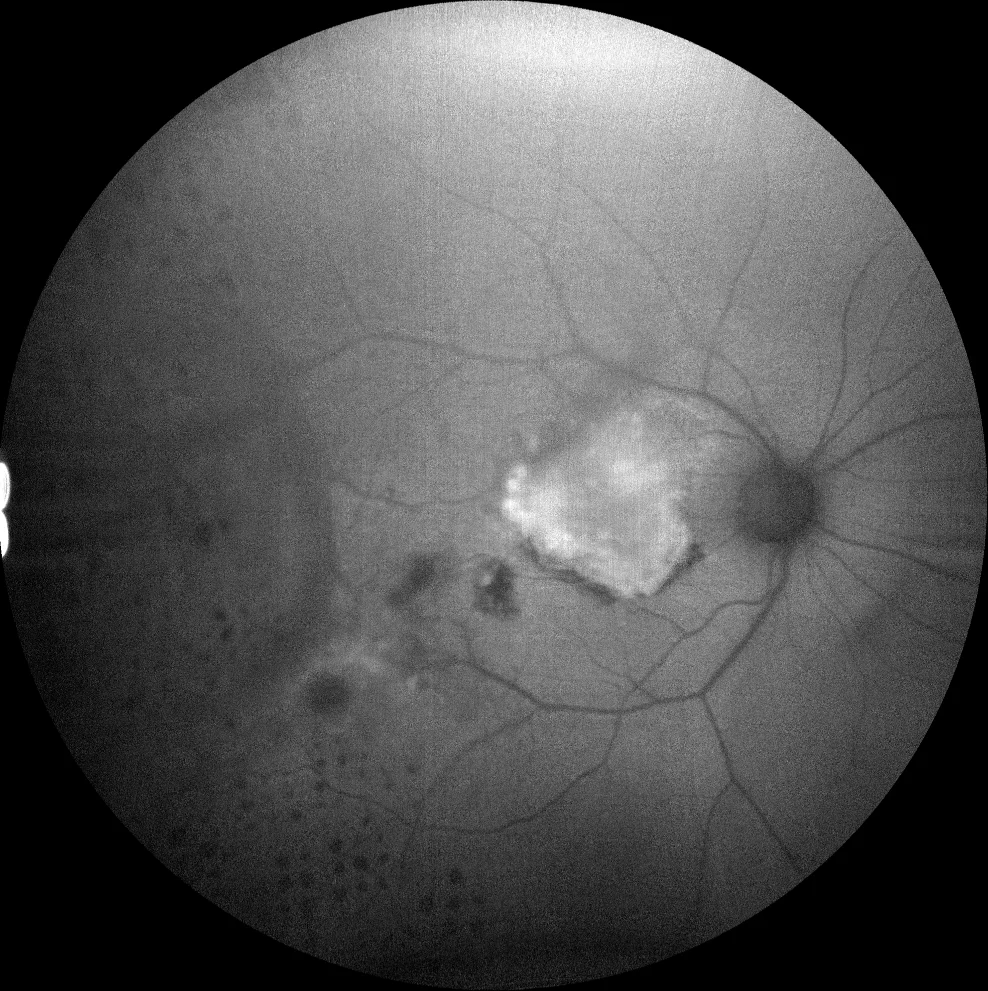
B. Autofluorescence image (Clarus 500, Carl Zeiss Meditec ASG, Jena, Germany) of the RE showing hyperautofluorescence of macular exudates, together with hypoautofluorescent panphotocoagulation scars temporally.
Description
Coats disease is an idiopathic retinal vasculopathy characterized by telangiectasias and retinal aneurysms and intra- and subretinal exudation. It typically affects males and young patients. It is almost always unilateral. Its etiology is unknown, although its pathophysiology involves ischemia, increased vascular endothelial growth factor (VEGF), increased vascular permeability, disruption of the blood-retinal barrier and finally exudation. Exudation produces the typical signs of the disease: intra- and subretinal fluid, lipid exudates and exudative retinal detachment.
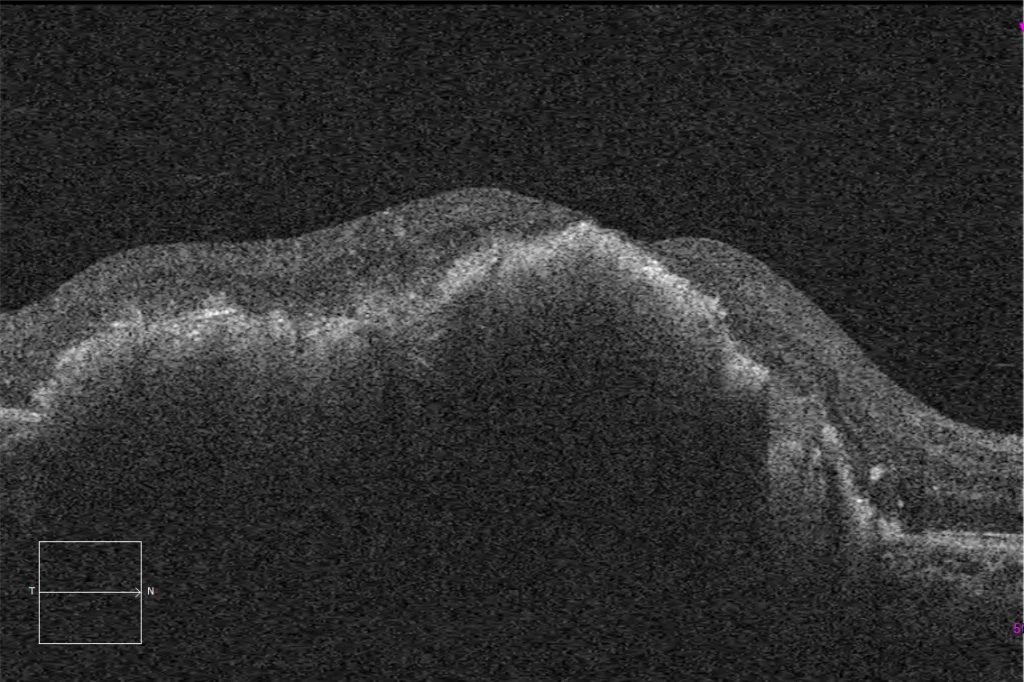
Multimodal imaging tests play an important role in the diagnosis. The most striking sign in the fundus is a profuse exudation with a lipid component. Fluorescein angiography can show areas of ischemia with capillary closure and leakage in the areas of exudation, although the most characteristic finding is bulb-like aneurysms. OCT shows intra- or subretinal fluid in the active phases, with other findings being hyperreflective points. The treatment in this case, as is common in patients with Coats disease, consisted of intravitreal injections with anti-VEGF drugs, intravitreal corticosteroids and argon laser photocoagulation of the affected areas, with the aim of producing impacts on the altered vessels (telangiectasias and aneurysms) and on the areas of ischemia due to capillary closure.