Diffuse Choroidal Atrophy
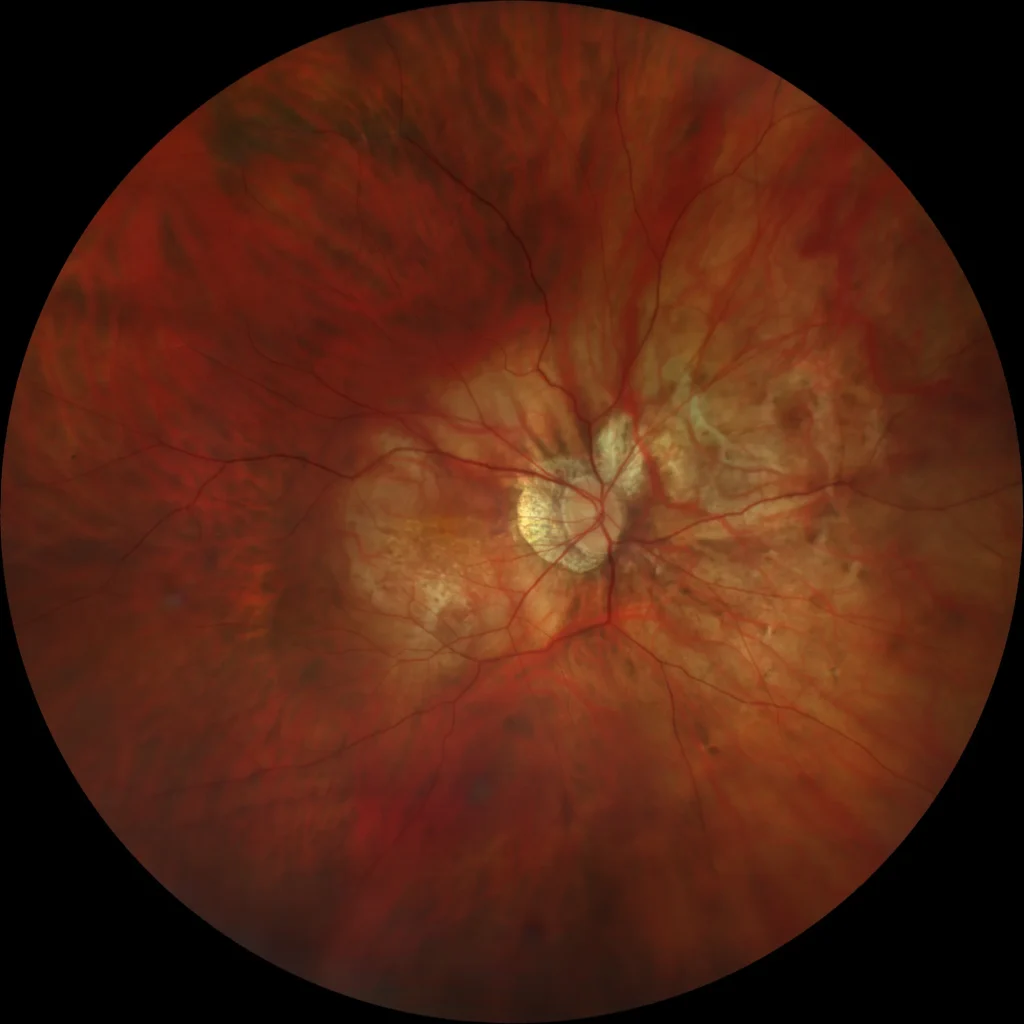
OD: Diffuse choroidal atrophy affecting the peripapillary area and posterior pole. Peripapillary chorio-retinal atrophy.
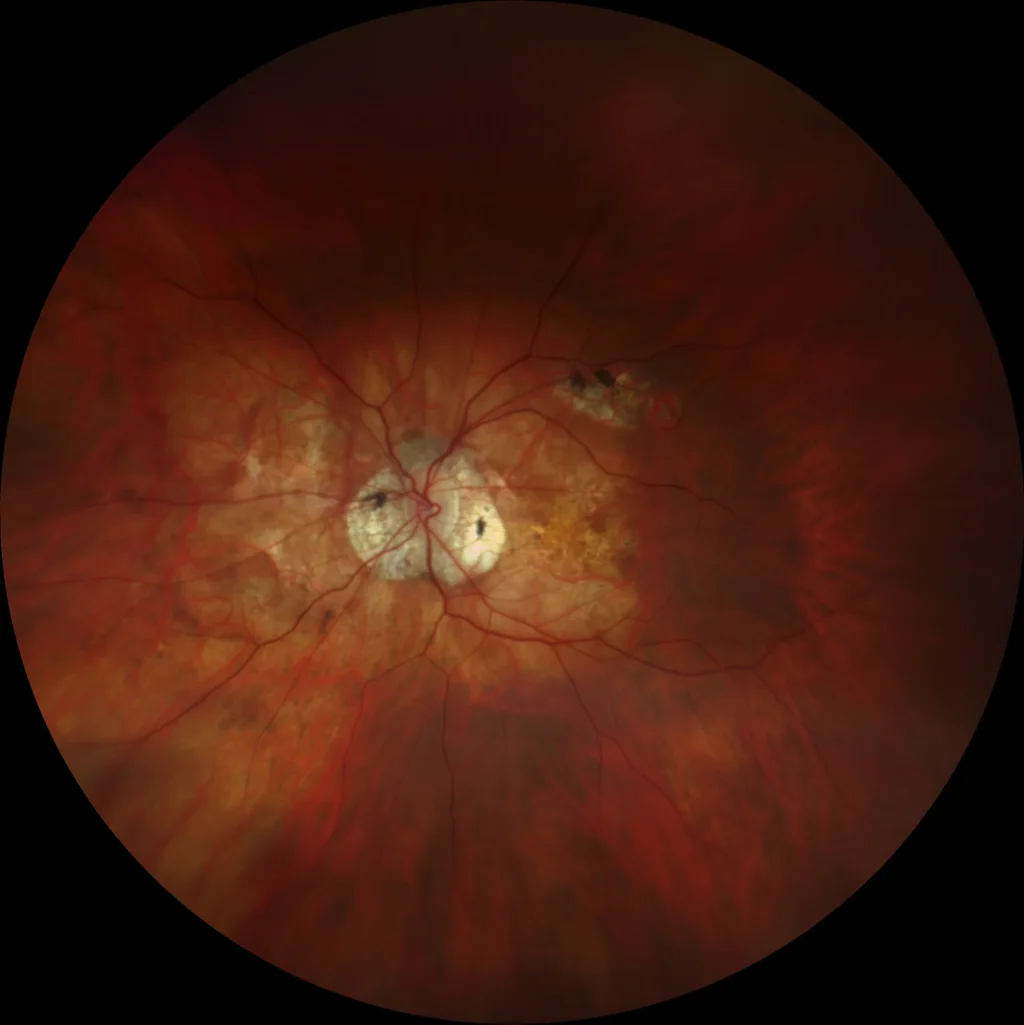
OS: Diffuse choroidal atrophy affecting the peripapillary area and posterior pole with granular pigmentary alteration in the macula. Peripapillary and superior to macular chorio-retinal atrophy plaques.
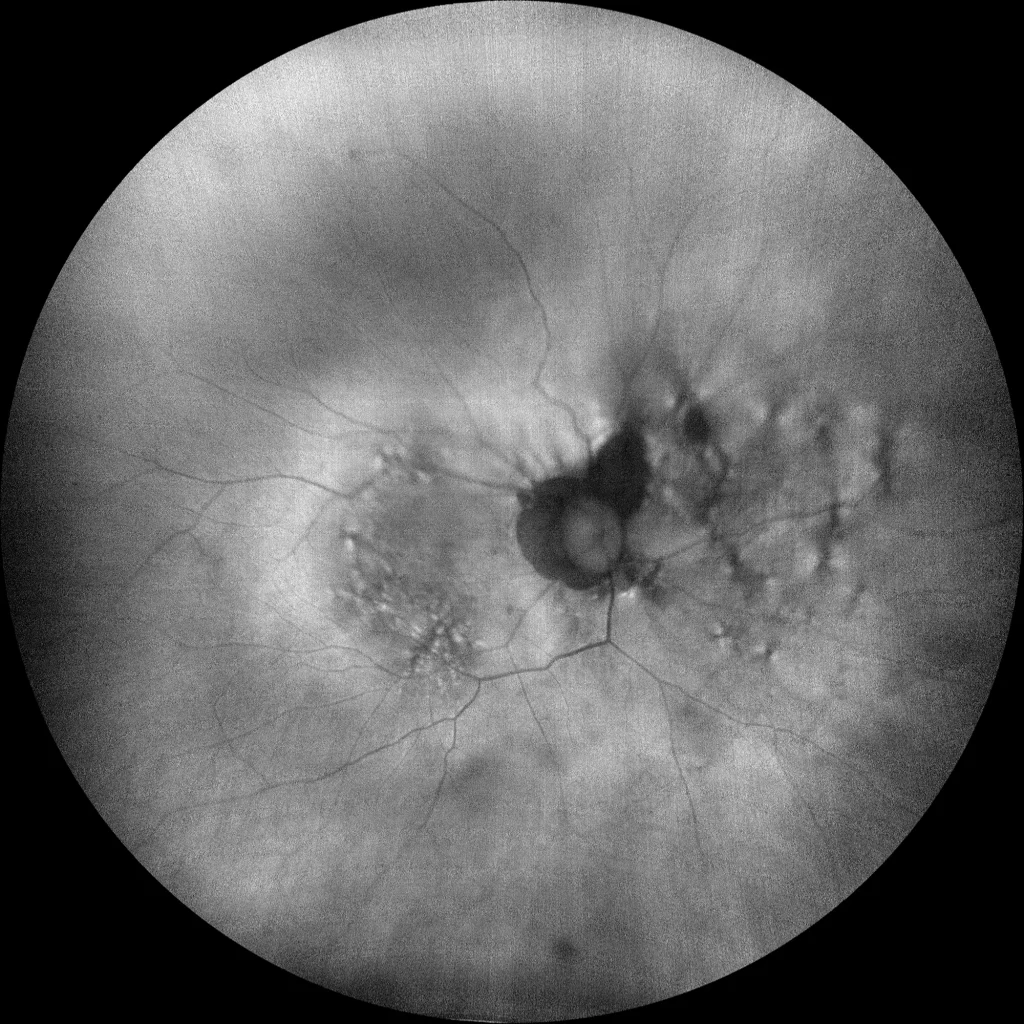
OD: The autofluorescence shows a fairly well-preserved posterior pole despite diffuse choroidal atrophy with mild perifoveal granular pigmentary alteration and a hypoautofluorescent peripapillary chorio-retinal atrophy plaque.
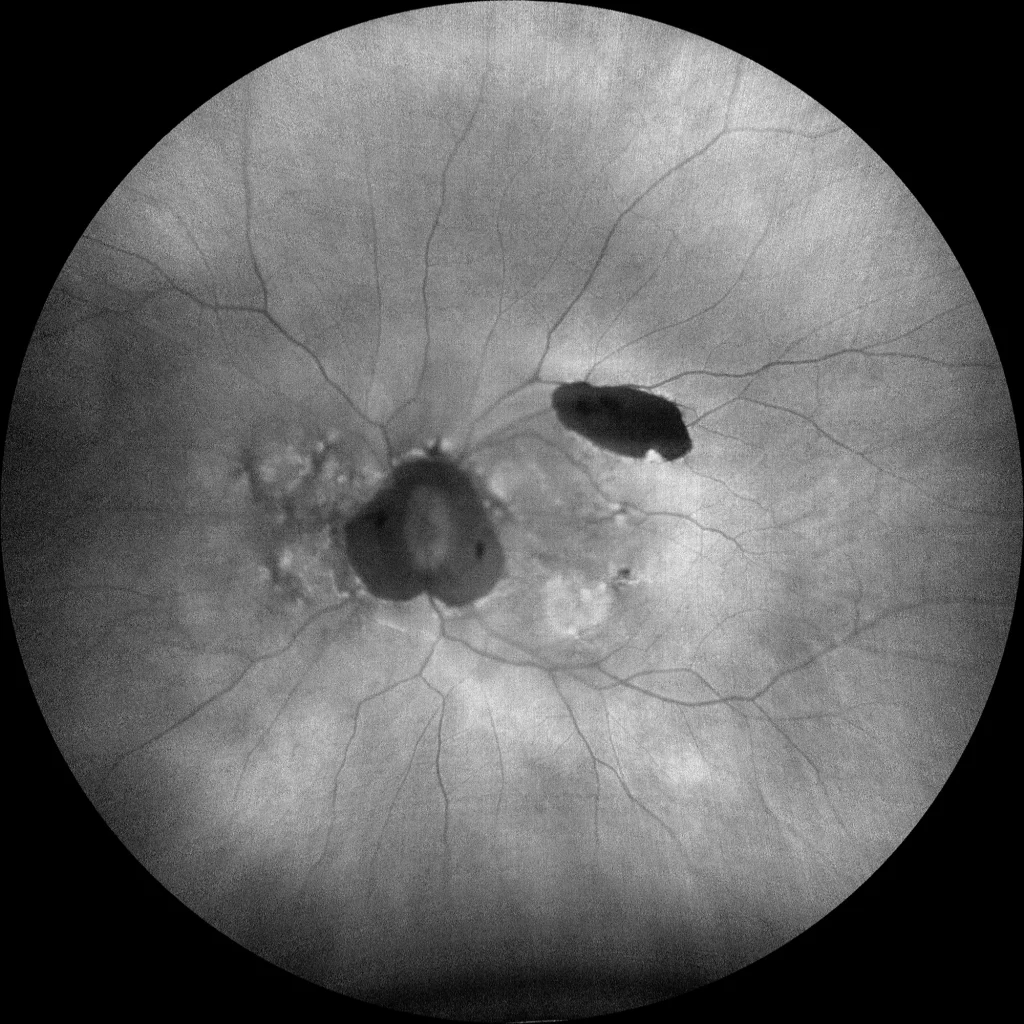
OS: Slight peripapillary and macular granular pigmentary alteration. The peripapillary and superior to macular chorio-retinal atrophy plaques appear hypoautofluorescent.
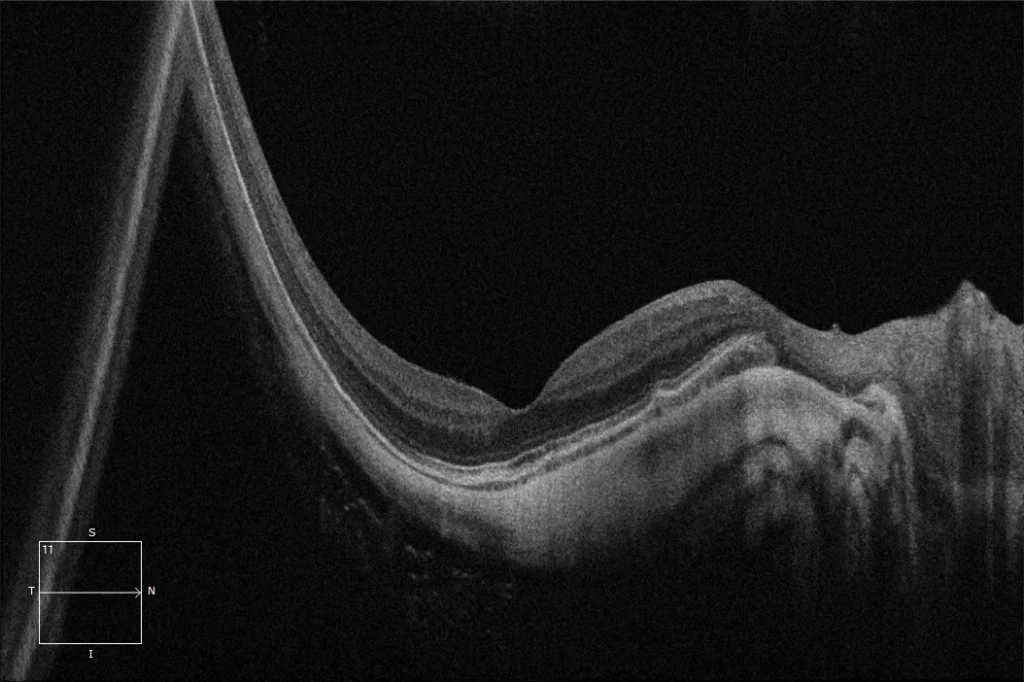
OD: Posterior staphyloma. Despite presenting marked choroidal thinning, it maintains a good foveal profile with a well-preserved outer retina.
Description
It corresponds to category 2 of the ATN classification of myopic atrophic maculopathy. It presents as a poorly defined yellowish lesion in the posterior pole of high myopes, which is not uniform and may have a granular appearance. It usually begins around the optic nerve and progresses to affect the entire posterior pole, and unlike tessellated fundus, the frequency of this lesion increases with age and axial length, being more prevalent above 40 years (30-52.9%) and above 28.5 mm of axial length (62.8%). On OCT, marked choroidal thinning can be observed; however, the retina and RPE are usually preserved, which could explain relatively preserved vision in these patients.
Comments
Minimum attached tests: Retinography + Autofluorescence + OCT- Color retinography (Clarus500, Zeiss): (A) OD: Diffuse choroidal atrophy affecting the peripapillary area and posterior pole. Peripapillary chorioretinal atrophy. (B) OS: Diffuse choroidal atrophy affecting the peripapillary area and posterior pole with granular pigmentary alteration in the macula. Peripapillary and superior to the macula chorioretinal atrophy plaques.
- Autofluorescence (Clarus500, Zeiss): (C) OD: The autofluorescence shows a fairly well-preserved posterior pole despite diffuse choroidal atrophy with mild perifoveal granular pigmentary alteration and a hypoautofluorescent peripapillary chorio-retinal atrophy plaque. (D) OS: Slight peripapillary and macular granular pigmentary alteration. The peripapillary and superior to macular chorio-retinal atrophy plaques appear hypoautofluorescent.
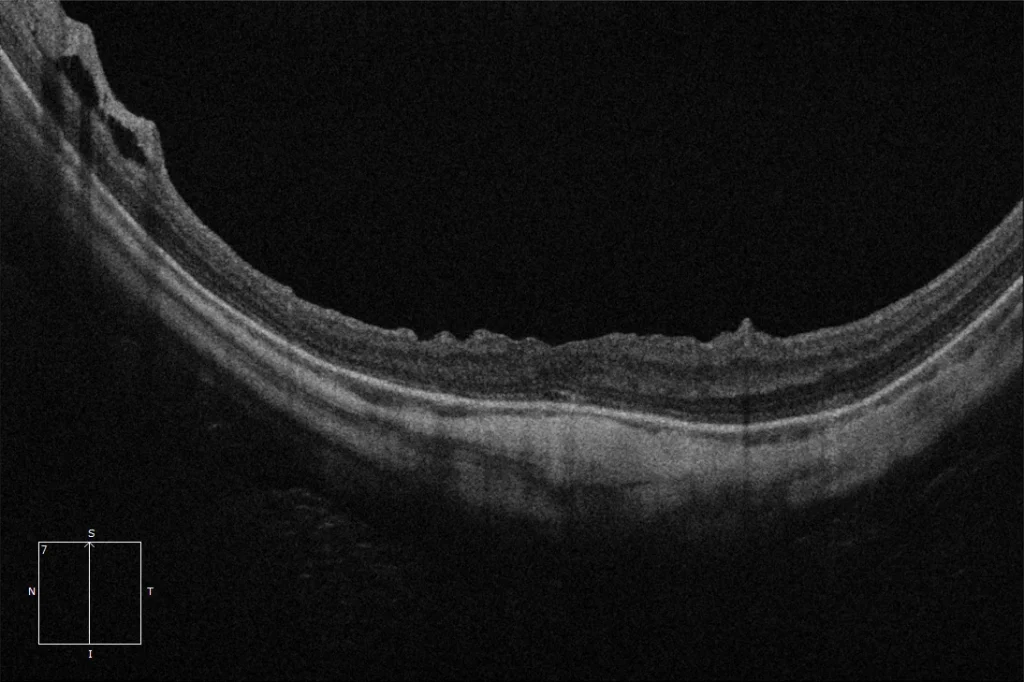
- OCT (Cirrus6000, Zeiss) (E) OD: Posterior staphyloma. Despite presenting marked choroidal thinning, it maintains a good foveal profile with a well-preserved outer retina. (F) OS: Posterior staphyloma. Marked choroidal thinning. Signs of macular surgery with internal limiting membrane peeling are observed with some DONFL (dissociated optic nerve fiber layer) in the inner retina. Some preservation of the outer retina is observed at the foveal level.