Internal punctate chorioretinopathy (IPC)
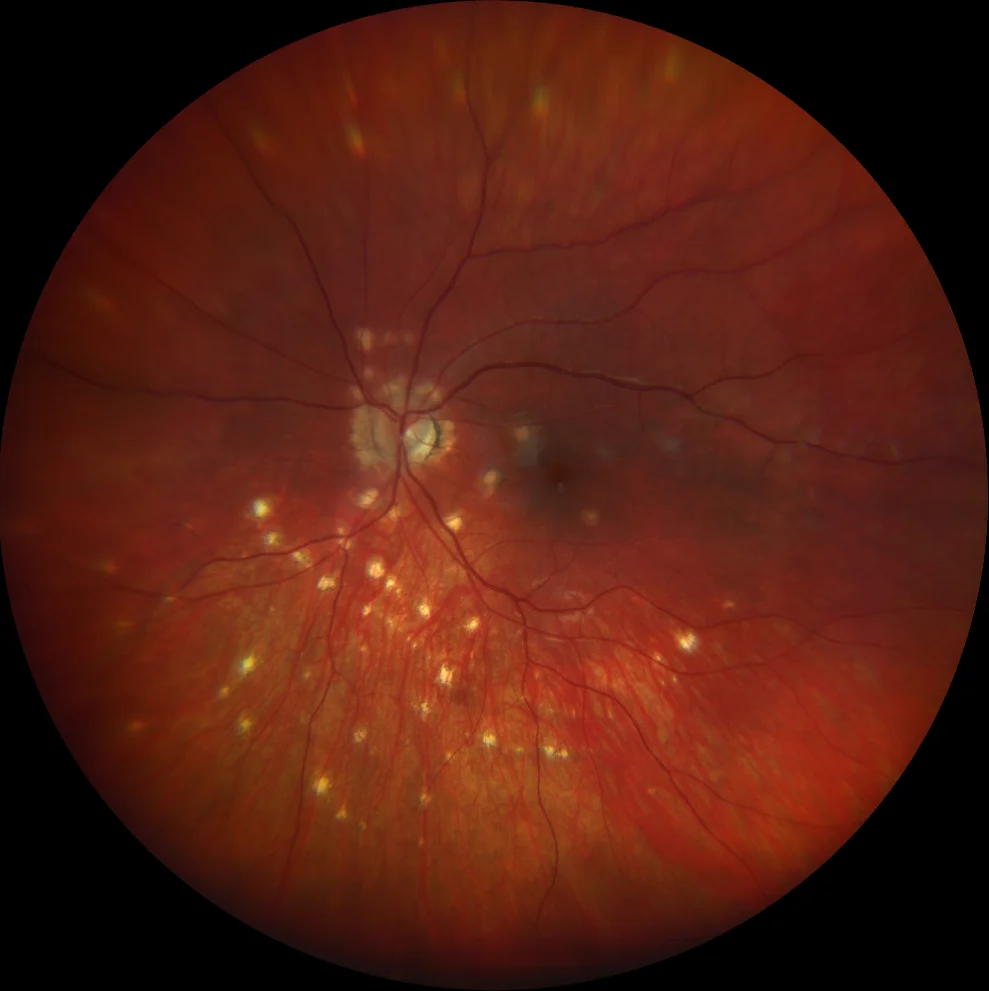
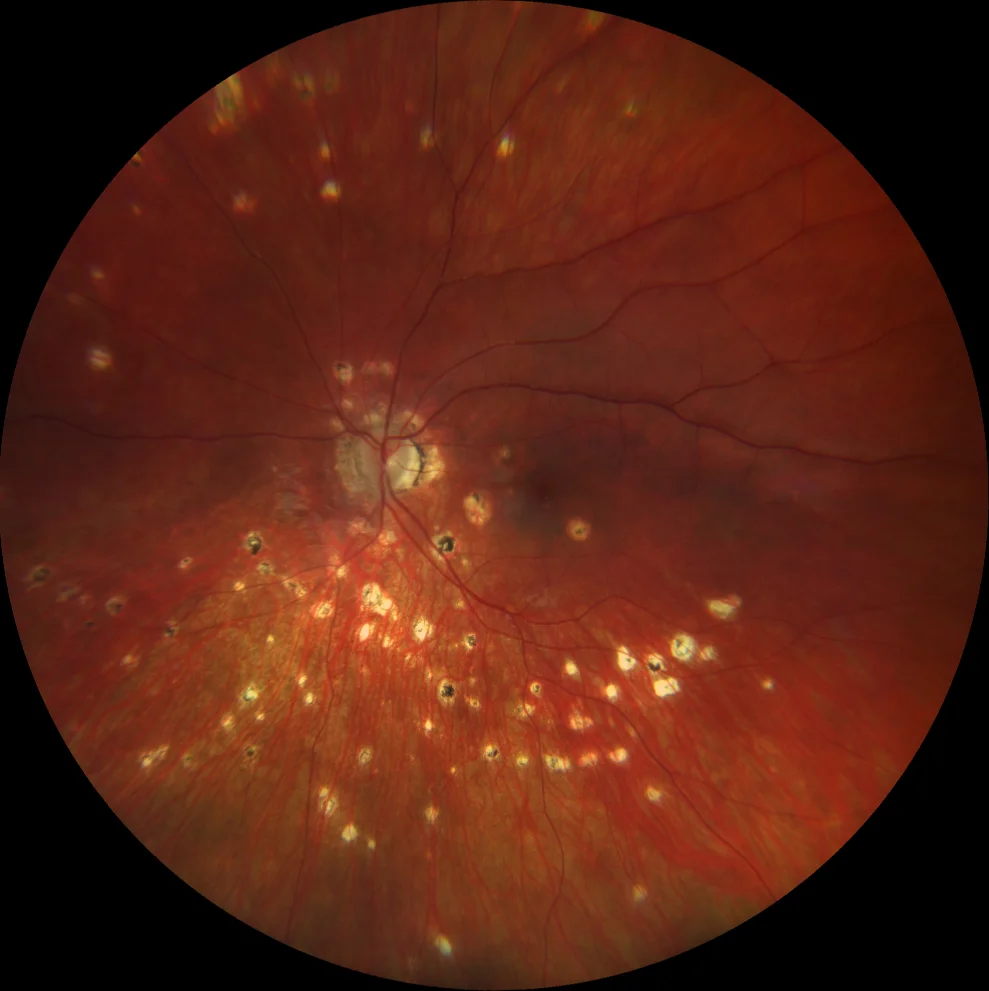
Retinography (Clarus 700, Zeiss): multiple yellowish punched-out lesions scattered around the periphery, peripapillary atrophy and 2 lesions in the macula similar to the peripheral ones, but with a grayish halo
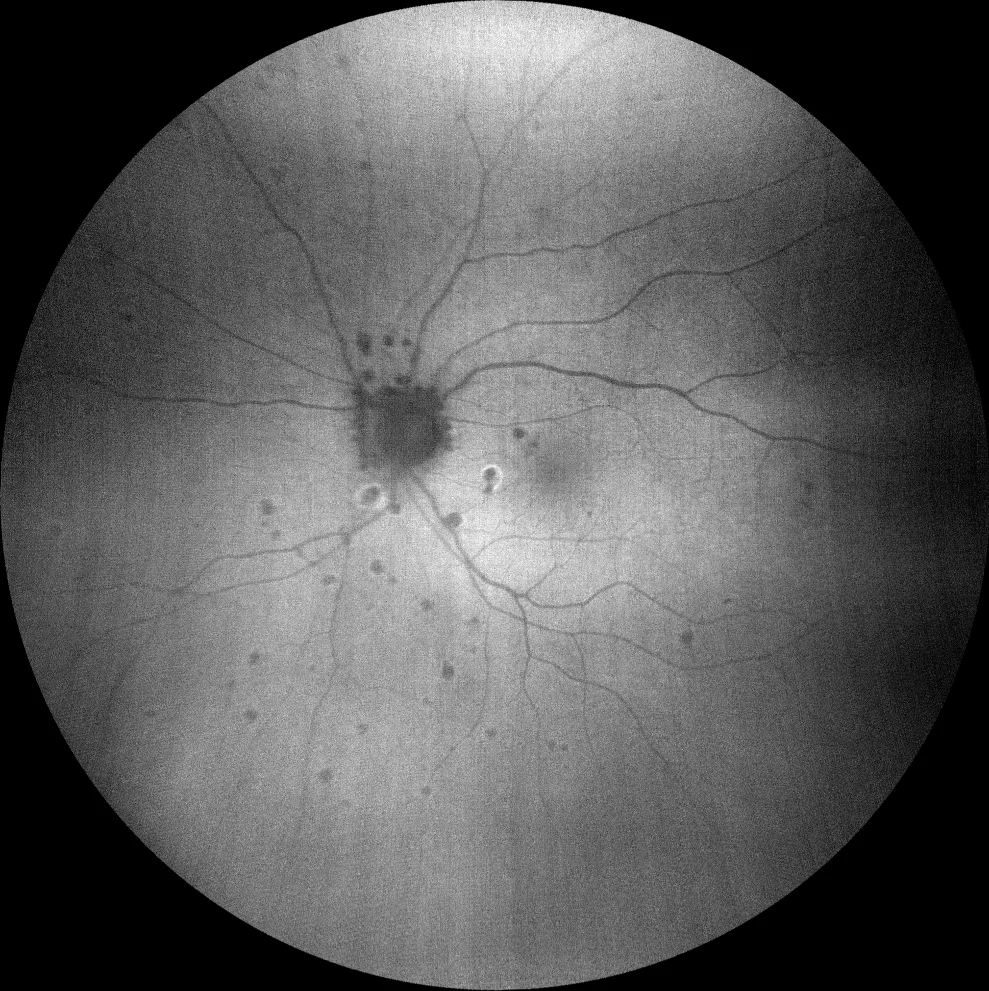
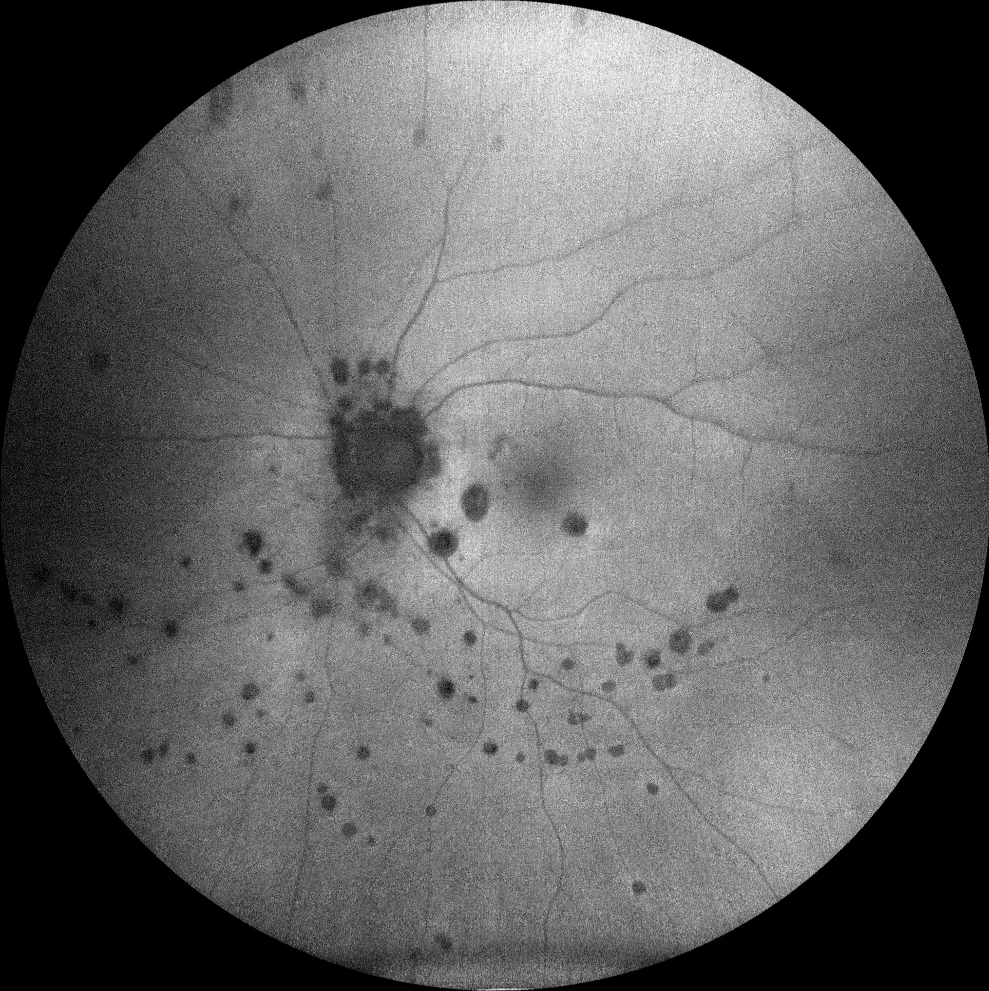
Green autofluorescence (Clarus 700, Zeiss): The peripheral lesions are hypoAF, revealing their atrophic nature. Of the 2 macular lesions, only the lower one presents a hyperAF halo. There is also another lesion with a lower juxtapapillary hyperAF halo.
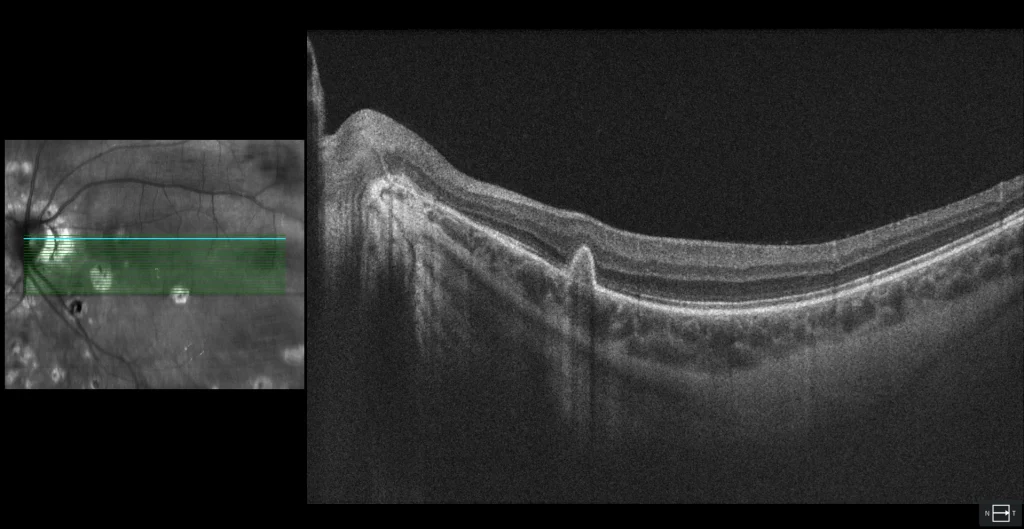
After 3 years of follow-up, it was observed that not only the number of lesions, but also their size, had increased.
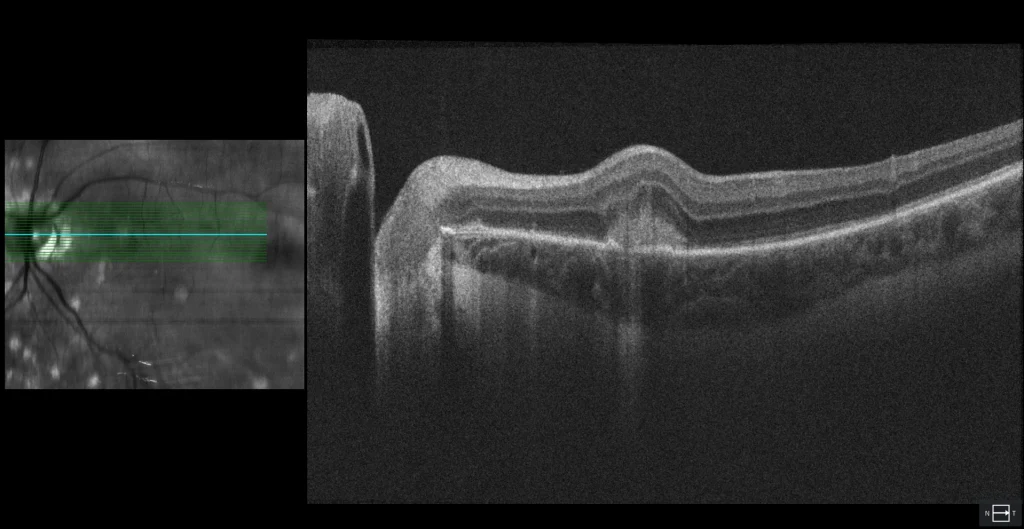
OCT (Cirrus 5000, Zeiss): MHSR with finger-like projections towards the inner retina, which is known as pitchfork sign and suggests inflammatory NVM
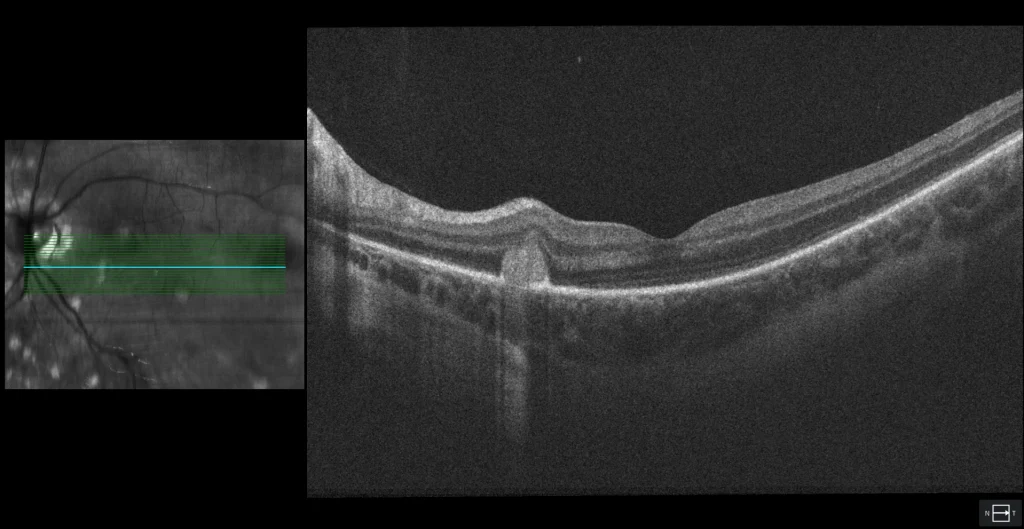
Macular lesion with hyperAF halo appears as well-defined, rounded MHSR with a break in continuity in the RPE, suggesting a focus of active choroiditis.
Description
21-year-old woman with a history of myopia (spherical equivalent -6.00 AO) who presents with flashes and blurred vision in the left eye, in addition to headache.
The VA is OD 20/25 and OI 20/25.
There are no inflammatory signs in the anterior pole or vitritis. The fundus shows multiple rounded, greyish-yellowish, punched-out lesions scattered around the periphery, as well as peripapillary atrophy and 2 lesions in the macula similar to the peripheral ones, but with a greyish halo. Of these lesions, the upper one shows hypoautofluorescence (hypoAF) (similar to the rest of the peripheral lesions) and on OCT it appears as an irregular subretinal hyperreflective material (SRHM) with finger-like projections towards the inner retina, suggesting that it is an inflammatory macular neovascularization (NVM). The other macular lesion with a halo is also hypoAF but with a hyperautofluorescent (hyperAF) halo; on OCT it appears as a rounded SRHM on a break in the RPE, suggesting a focus of inflammatory choroiditis. The diagnosis of internal punctate choroidopathy (IPC) is made. Intravitreal antiangiogenic treatment and oral corticosteroids were recommended, but the patient refused. Four months later, the patient reported blurred vision; oral prednisone was prescribed at a dose of 1 mg/kg weight/day, but the patient discontinued the treatment. After 3 years of follow-up, the number of punched-out lesions was observed to have increased, although there was no recurrence of either the inflammatory lesions or the inflammatory VAP. The latter was enveloped by the RPE.