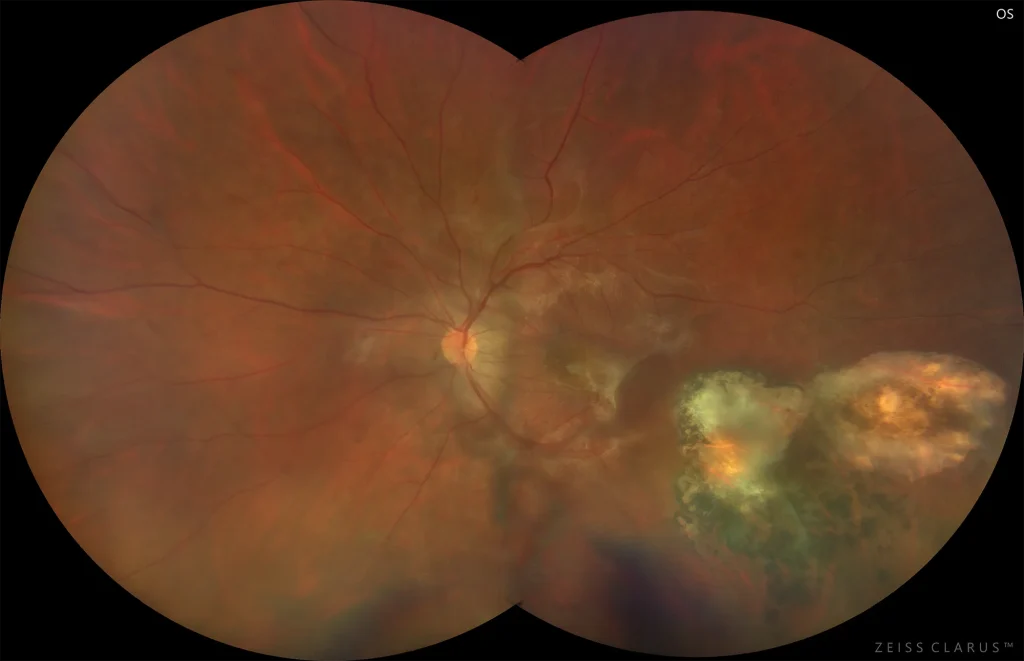
Macular epiretinal membrane in a patient with toxoplasmosis
Figure 1. Color retinography showing an epiretinal membrane at the macular level and a pigmented temporal inferior chorioretinal scar secondary to toxoplasmosis
Description
Toxoplasmosis is the most common cause of infectious retinochoroiditis in humans. Characteristic features include a pigmented retinochoroidal scar, focal necrotizing granulomatous retinitis, reactive granulomatous choroiditis, vitritis, and even inflammatory activity in the anterior segment. Treatment is not always necessary; this will depend on the patient’s immune status, the location of the lesion, the degree of vitritis, or the clinical course, among others.
There are different combinations of treatments, the most commonly used being the combination of trimethoprim-sulfamethoxazole or pyrimethamine with folinic acid and with sulfadiazine and/or clindamycin. Prednisone can be associated with these treatments. An alternative option is intravitreal injections of clindamycin and dexamethasone.
One of the complications secondary to this pathology is the appearance of an epiretinal membrane that can be treated surgically after three months without signs of intraocular inflammation.