Posterior Staphyloma
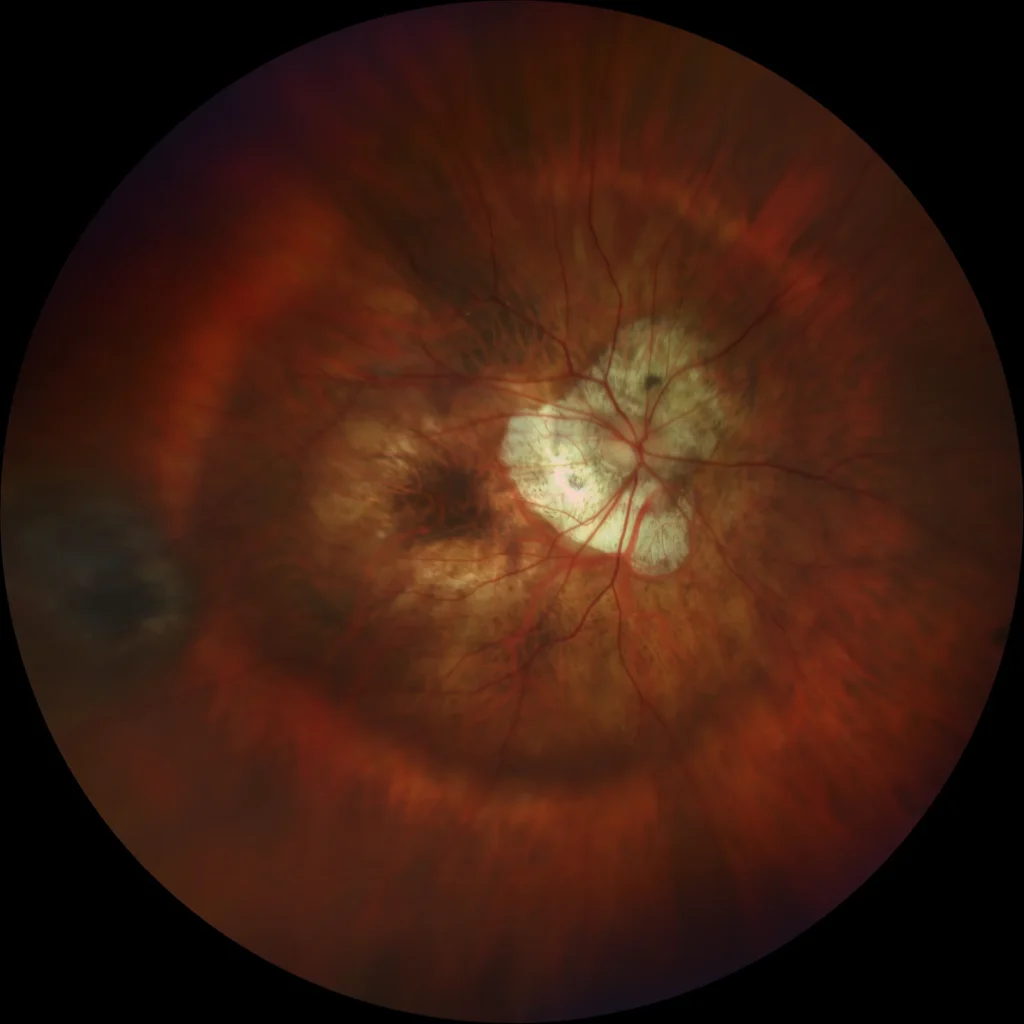
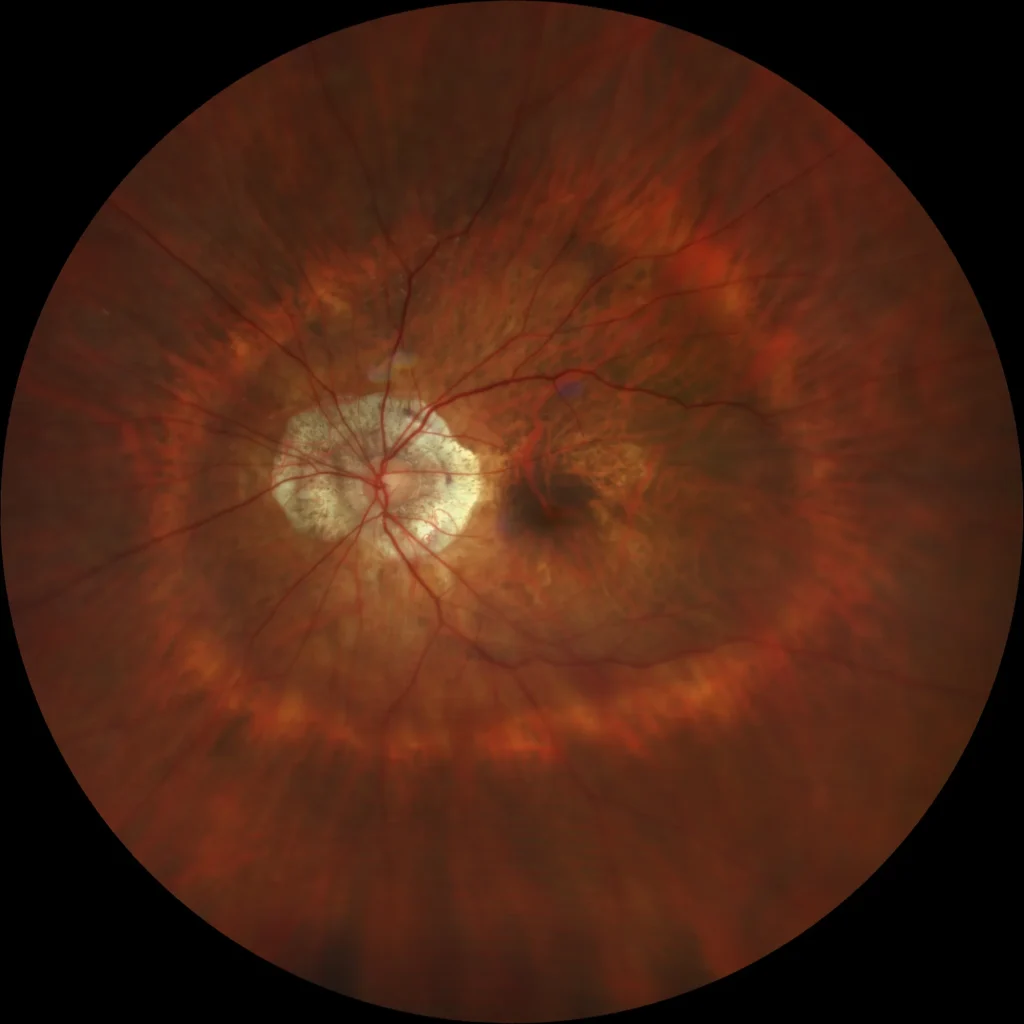
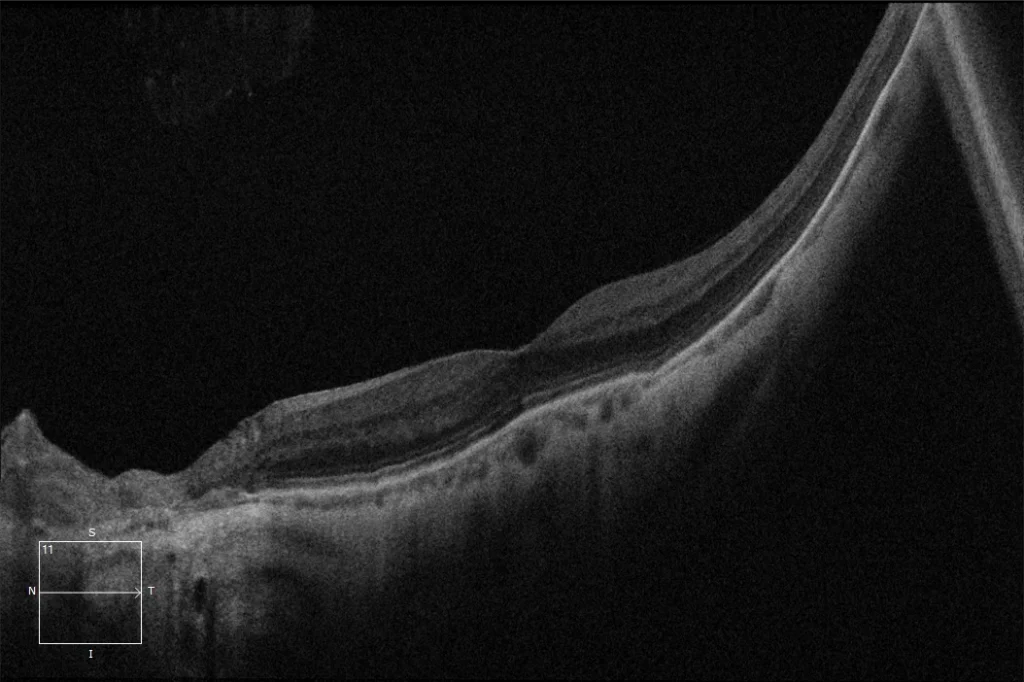
BE: Wide macular staphyloma (type I). The border of the staphyloma is observed outside the posterior pole (outside vascular arcades) and nasal to the optic nerve. Peripapillary chorioretinal atrophy.
BE: Wide macular staphyloma (type I). The border of the staphyloma is observed outside the posterior pole (outside vascular arcades) and nasal to the optic nerve. Peripapillary chorioretinal atrophy.
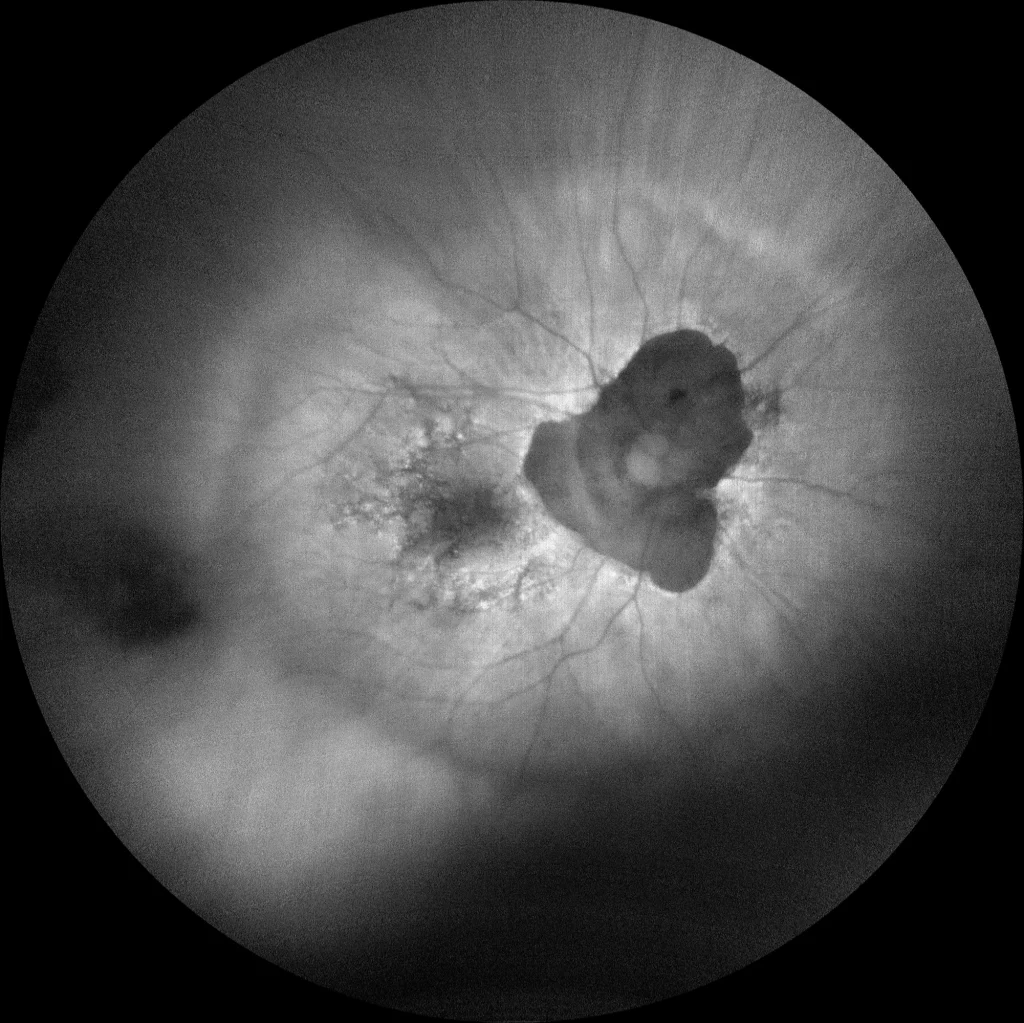
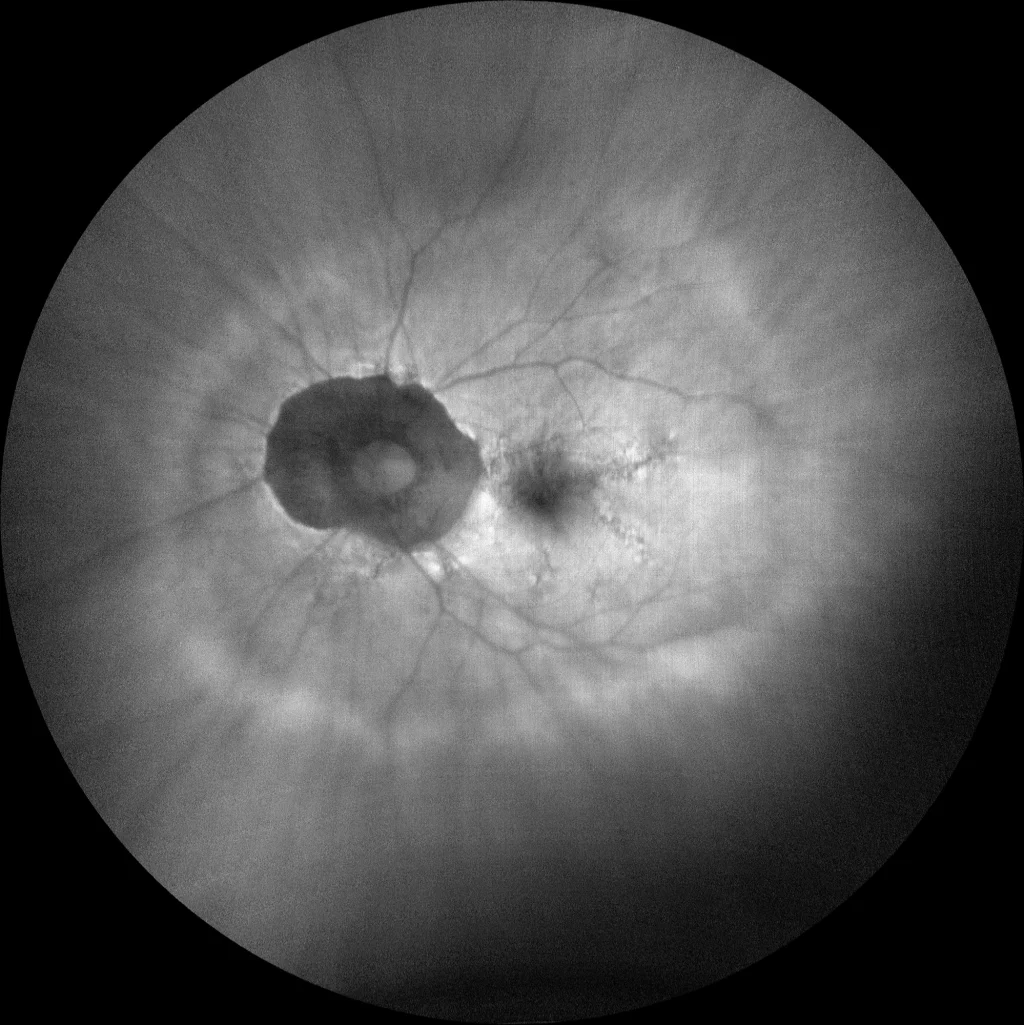
BE: Wide macular staphyloma. In autofluorescence, the borders of the staphyloma can be delineated, as well as the chorioretinal atrophy plaques (peripapillary hypoautofluorescence area). We can also observe pigmentary changes at the macular level in the form of granular hypo and hyperautofluorescence.
BE: Wide macular staphyloma. In autofluorescence, the borders of the staphyloma can be delineated, as well as the chorioretinal atrophy plaques (peripapillary hypoautofluorescence area). We can also observe pigmentary changes at the macular level in the form of granular hypo and hyperautofluorescence.
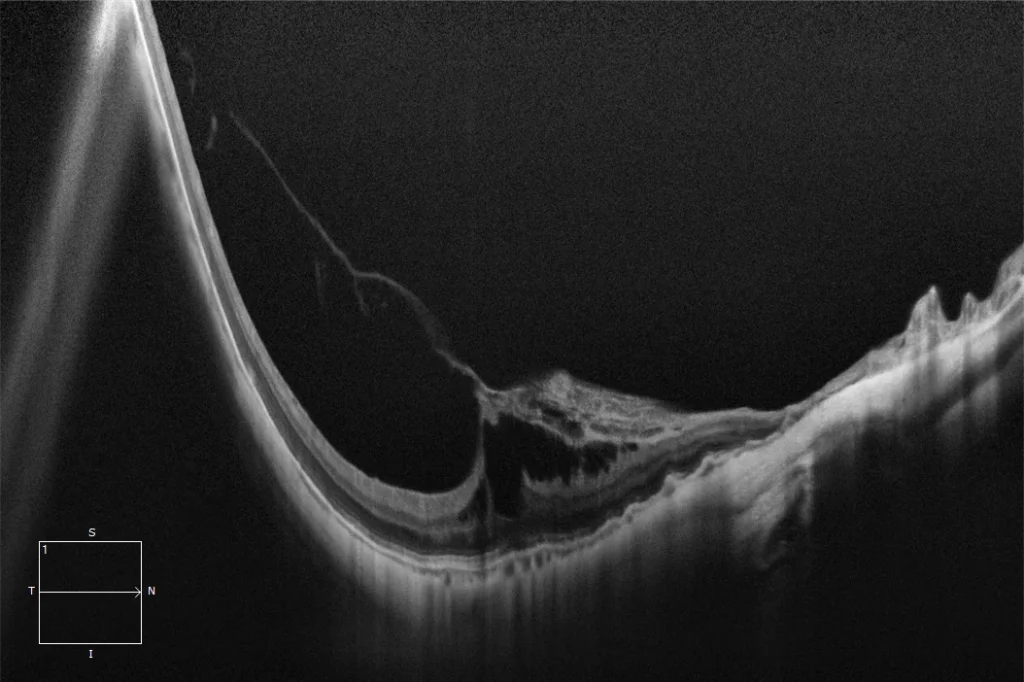
RE: Posterior staphyloma with vitreomacular traction. Appears to have avulsion of part of the inner retina and mild foveoschisis due to vitreomacular traction.
Description
Posterior staphyloma is the most characteristic sign and the main marker of pathological myopia. Spaide defined it as an evagination or protrusion of the ocular wall that has a radius of curvature smaller than that of the surrounding curvature of the eye wall. This definition was intended to differentiate staphyloma from a simple uniform elongation of the eyeball backwards.
Its prevalence varies depending on two factors: age and axial length.
There is a clear association between posterior staphyloma and many of the characteristic lesions of high myopia (chorioretinal atrophy, myopic tractional maculopathy, myopic neovascular membranes, visual field defects, etc.) that can lead to loss of visual acuity.
The most recent classification is by Ohno-Matsui and divides posterior staphylomas into:
- Type I: Wide macular staphyloma
- Type II: Narrow macular staphyloma
- Type III: Peripapillary staphyloma
- Type IV: Nasal staphyloma
- Type V: Inferior staphyloma
- Others